Putting alcohol and sleep medications together isn’t just a bad idea-it’s a life-threatening one. You might think having a glass of wine to help you unwind before taking your prescription sleep aid is harmless. Maybe you’ve even heard someone say, "It helps me fall asleep faster." But the truth is, this combo doesn’t just make you drowsy. It can shut down your breathing, cause you to drive while asleep, or even kill you-without you ever realizing what’s happening.
How Alcohol and Sleep Medications Work Together
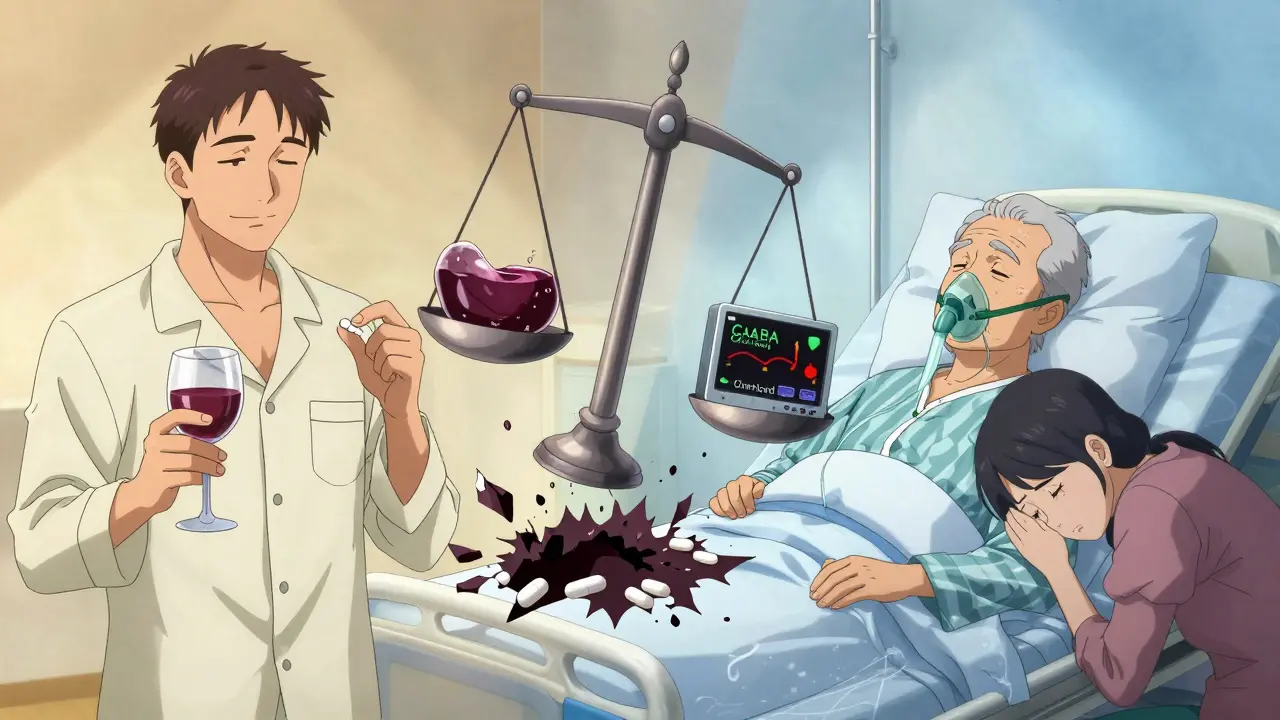
Both alcohol and sleep medications like Ambien, Lunesta, and Klonopin slow down your central nervous system. They do this by boosting the effects of a brain chemical called GABA, which tells your brain to calm down. When you take one, it’s noticeable but manageable. When you mix them, it’s not just double the effect-it’s exponential.Think of it like stacking weights on a scale. One weight might press down gently. Add another, and the scale bends more. But if those two weights are magnetically pulled together, the pressure spikes far beyond what either could do alone. That’s what happens with alcohol and Z-drugs like zolpidem (Ambien). A 2021 study from the University of California San Francisco found that even a tiny amount of alcohol-just 0.02% blood alcohol concentration, equal to one drink-slowed how fast Ambien leaves your body. Instead of clearing in 2.5 hours, it lingers for over six. That means you’re sedated longer, deeper, and more dangerously than you ever intended.
And it’s not just Ambien. Eszopiclone (Lunesta) combined with alcohol at the legal driving limit (0.08% BAC) dropped oxygen levels in the blood to 84.7%. Normal is above 92%. Breathing slowed from 16 breaths per minute to 9.3. That’s not sleepy-that’s medically critical.
Which Sleep Medications Are Most Dangerous With Alcohol?
Not all sleep meds are the same when mixed with alcohol. The risk varies by type:- Z-drugs (Ambien, Lunesta, Sonata): These are the worst offenders. They act fast, bind tightly to brain receptors, and dramatically amplify alcohol’s depressant effects. In 2022, the FDA reported that Ambien-alcohol combinations caused 63% of all emergency visits related to sleep meds and alcohol-even though Ambien is only prescribed about 38% of the time.
- Benzodiazepines (Klonopin, Ativan, Restoril): These are older, still widely used, and dangerous too. They increase fall risk, confusion, and memory loss. When combined with alcohol, impairment in driving ability rises 1.9 times higher than alcohol alone.
- OTC sleep aids (ZzzQuil, Unisom): These contain diphenhydramine or doxylamine, antihistamines that make you drowsy. For older adults, mixing these with alcohol triples the risk of falling. Emergency room data shows hip fractures from this combo jumped from 12.7 to 51.3 per 100,000 seniors per year.
- Melatonin: This is the exception. It doesn’t act on GABA like the others. Mixing melatonin with alcohol doesn’t cause respiratory depression or fatal sedation. But it still makes you groggy the next day-up to 35% more drowsiness than alcohol alone.
The FDA now requires a Black Box Warning on all Z-drugs-the strongest safety alert they can issue-stating that combining them with alcohol is contraindicated. That’s medical code for: "Don’t do this. Ever."
Real People, Real Consequences
Behind the statistics are stories people don’t always talk about. On Reddit, users share chilling experiences: waking up miles from home with no memory of driving, finding themselves in strange places, or being found unconscious by family members.One user, u/SleepWalker99, posted in March 2023: "Took half an Ambien with two glasses of wine. Woke up two miles from home. No idea how I got there. My car was in the ditch. I didn’t even know I’d been driving." That’s not an anomaly. Clinical studies show the risk of sleep-driving-where you perform complex tasks while not fully awake-jumps from 0.15% with Z-drugs alone to 2.4% when alcohol is involved.
On Drugs.com, Ambien has a 1.8 out of 5-star safety rating when mixed with alcohol. The most common complaint? "Extreme drowsiness lasting 12+ hours." Lunesta users report confusion and memory loss in over half their negative reviews. For older adults, the consequences are even grimmer. In AARP forums, 73% of posts from seniors describe being hospitalized after mixing even one drink with OTC sleep aids.

Who’s Most at Risk?
It’s not just heavy drinkers or people who ignore warnings. The biggest group affected? Adults aged 35 to 54. They’re the most likely to be prescribed sleep meds, and they’re also the most likely to have a drink at night. According to national ER data, this group makes up over half of all alcohol-sedative emergency visits.But the most severe outcomes? They happen to older adults. Why? Because as we age, our livers process alcohol and drugs slower. That means both substances stay in the system longer, increasing the risk of overdose. A 65-year-old who drinks one glass of wine and takes a sleep pill isn’t just risking drowsiness-they’re risking respiratory failure.
And here’s the kicker: 68% of people prescribed sleep meds say they were never properly warned about alcohol risks. Even though 92% of sleep specialists know the danger, that knowledge doesn’t always reach the patient.
What Should You Do Instead?
If you’re using sleep meds and drinking alcohol, stop. Period. There’s no safe amount. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) says even one drink can be dangerous. Their guidelines recommend:- Wait at least 6 hours after your last drink before taking a Z-drug.
- Wait 12 hours if you’re on a benzodiazepine.
- Avoid alcohol completely if you’re over 65 and taking any sleep medication.
But the real solution? Don’t rely on pills at all. The American Medical Association now recommends treating insomnia with non-drug methods first: cognitive behavioral therapy for insomnia (CBT-I), better sleep hygiene, and reducing screen time before bed. These approaches work better long-term and carry zero risk of deadly interactions.
There’s also new hope in medication development. Dayvigo (lemborexant), approved in 2023, works differently-it blocks orexin, a brain chemical that keeps you awake. Unlike Z-drugs, it only increases its half-life by 15% when mixed with alcohol, not 150-200%. It’s not a magic fix, but it’s a step toward safer options.
What If You’ve Already Mixed Them?
If you’ve taken alcohol and a sleep med together and feel unusually sleepy, confused, or have trouble breathing, call 911 immediately. Don’t wait. Don’t try to sleep it off. Respiratory depression can happen fast and silently.If you’re worried you might have done this without realizing it-maybe you woke up somewhere strange or can’t remember part of the night-talk to your doctor. These episodes aren’t rare. They’re documented, preventable, and treatable if caught early.
Pharmacists are now required to hand out FDA-approved medication guides with every sleep prescription. These guides must include the warning: "Do not consume alcohol while taking this medication"-in bold, 14-point font. If you didn’t get one, ask for it. If your doctor didn’t mention it, ask them again.
Why This Isn’t Just About "Being Careful"
Some people think if they’re "light drinkers" or "only take half a pill," they’re safe. That’s a myth. A 2021 study in the American Journal of Psychiatry found that 83% of fatal Ambien-alcohol interactions happened at blood alcohol levels below the legal driving limit-0.051% on average. That’s less than one drink for most people.This isn’t about willpower. It’s about chemistry. Your body can’t tell the difference between a "small" amount of alcohol and a "big" one when it’s already dealing with a powerful CNS depressant. The interaction doesn’t care how careful you are. It only cares about the molecules in your bloodstream.
The FDA, CDC, and American Academy of Sleep Medicine all agree: there is no safe level of alcohol with prescription sleep aids. Not one sip. Not one glass. Not even one drink on a special night.
Sleep should help you rest-not put you in danger. If you’re struggling with insomnia, talk to your doctor about safer, non-drug options. Your life depends on it.
Can I have one drink with Ambien if I wait a few hours?
No. Even one drink combined with Ambien can dangerously slow your breathing and increase the risk of sleepwalking, memory loss, or overdose. The FDA and NIAAA state that no amount of alcohol is safe with Z-drugs like Ambien. Waiting 6 hours reduces but doesn’t eliminate the risk-especially if you’re over 35 or have liver issues.
Is it safer to use melatonin instead of prescription sleep meds with alcohol?
Melatonin doesn’t interact with alcohol in the same dangerous way as Ambien or Lunesta. It doesn’t suppress breathing or cause complex sleep behaviors. But it still increases next-day drowsiness by up to 35%. While not life-threatening, it can impair your ability to drive or work safely the next morning.
Why do older adults face higher risks with alcohol and sleep meds?
As we age, our liver processes alcohol and medications more slowly. This means both substances stay in the body longer, increasing sedation and fall risk. Adults over 65 who mix alcohol with OTC sleep aids like Unisom have a 300% higher chance of falling and fracturing a hip. The American Geriatrics Society recommends avoiding alcohol completely in this group.
Can I take sleep meds after drinking the night before?
If you drank heavily the night before, your body may still be processing alcohol. Even if you feel fine, alcohol can linger in your system for 12-24 hours. Taking a sleep med while alcohol is still present increases sedation risk. Wait at least 12 hours after your last drink before taking benzodiazepines, and 6 hours for Z-drugs-but ideally, avoid the combination entirely.
What should I do if I think I’ve had a sleep-driving episode?
If you’ve woken up somewhere you don’t remember driving to, or found yourself in a strange situation after taking sleep meds and alcohol, stop using both immediately. Contact your doctor and mention the episode. These events are a sign of dangerous CNS depression. Your doctor may switch you to a non-GABA medication like Dayvigo or recommend CBT-I for long-term sleep improvement.

