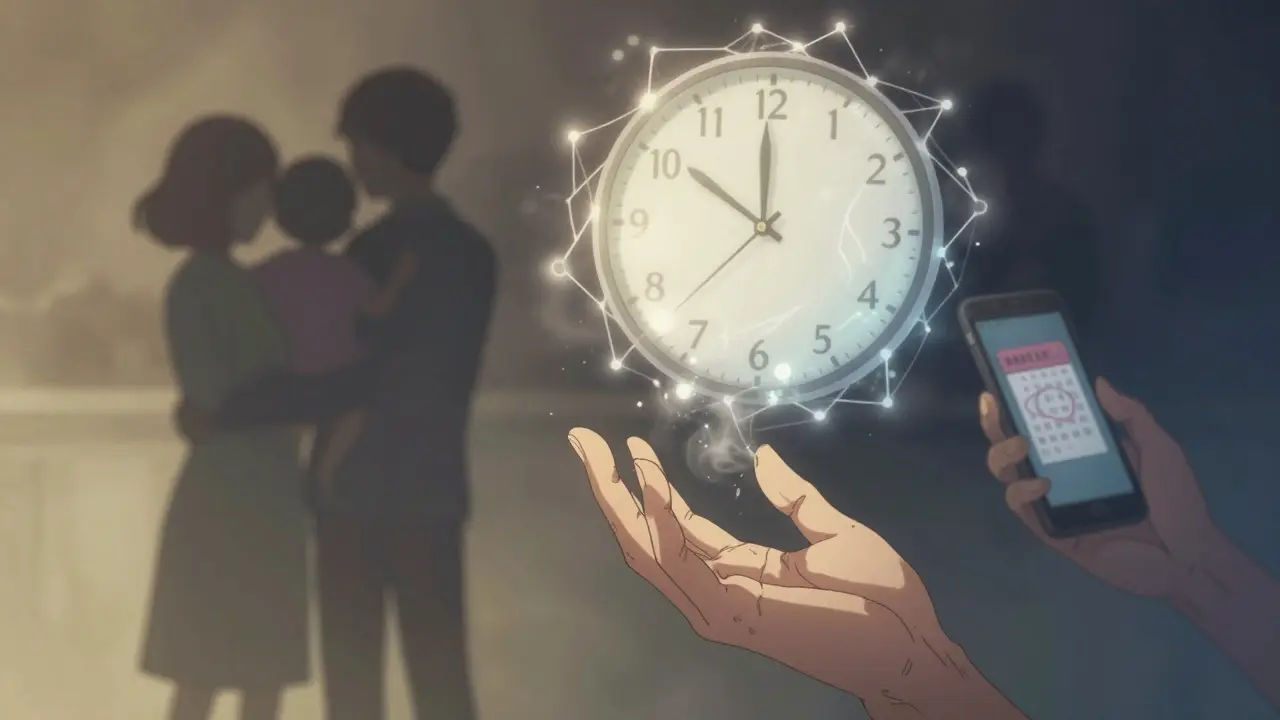
ALS doesn’t come with warning signs. One day, you might notice your foot dragging, or your hand feels weaker when holding a coffee cup. The next, you’re struggling to speak clearly or swallow food. There’s no cure. No magic fix. Just a slow, relentless loss of movement, strength, and control - all because the nerves that tell your muscles to work are dying. This is amyotrophic lateral sclerosis, or ALS, also known as Lou Gehrig’s disease. It affects about 2 in 100,000 people each year. Most people live 3 to 5 years after symptoms start. But for some, a small, old drug called riluzole offers a fragile kind of hope - not a cure, but a few extra months.
What Happens When ALS Takes Over
ALS attacks the motor neurons - the nerve cells in your brain and spinal cord that send signals to your muscles. When these neurons die, your muscles stop receiving messages. They weaken. They twitch. They waste away. It starts in one place - maybe your hand, your leg, or your voice - and spreads. Eventually, you lose the ability to walk, talk, eat, and breathe on your own. The mind stays sharp. The pain is usually mild. But the helplessness? That’s what haunts patients and families.There’s no single test for ALS. Doctors rule out other conditions - multiple sclerosis, spinal stenosis, Lyme disease - before landing on the diagnosis. Electromyography (EMG), nerve conduction studies, and MRI scans help confirm the pattern of nerve damage. Blood and spinal fluid tests rule out mimics. By the time most people are diagnosed, the disease has already been working for months, maybe even years.
Riluzole: The First Drug That Gave ALS Patients a Chance
For over 20 years, riluzole was the only drug approved to slow ALS progression. It hit the market in 1995, after decades of failed experiments. Before riluzole, there was nothing. Just supportive care - feeding tubes, ventilators, physical therapy - all aimed at comfort, not control.Riluzole doesn’t stop ALS. It doesn’t reverse damage. But it does something no other drug had done before: it slightly delays death. In the landmark 1996 trial with nearly 1,000 patients, those taking riluzole had a 35% lower risk of dying or needing a tracheostomy within 18 months. The average survival gain? Two to three months. Sounds small. But in a disease where time is measured in weeks, those months matter. They mean one more birthday. One more hug. One more conversation.
It works by targeting glutamate, a chemical messenger in the brain. Too much glutamate overstimulates nerve cells, causing them to burn out - a process called excitotoxicity. Riluzole blocks the release of glutamate and dampens its effects on nerve receptors. It also shuts down sodium channels in nerve endings, which helps calm overactive signaling. But here’s the frustrating part: scientists still don’t fully understand how it works. Other drugs that target glutamate failed. Riluzole somehow does more than that.
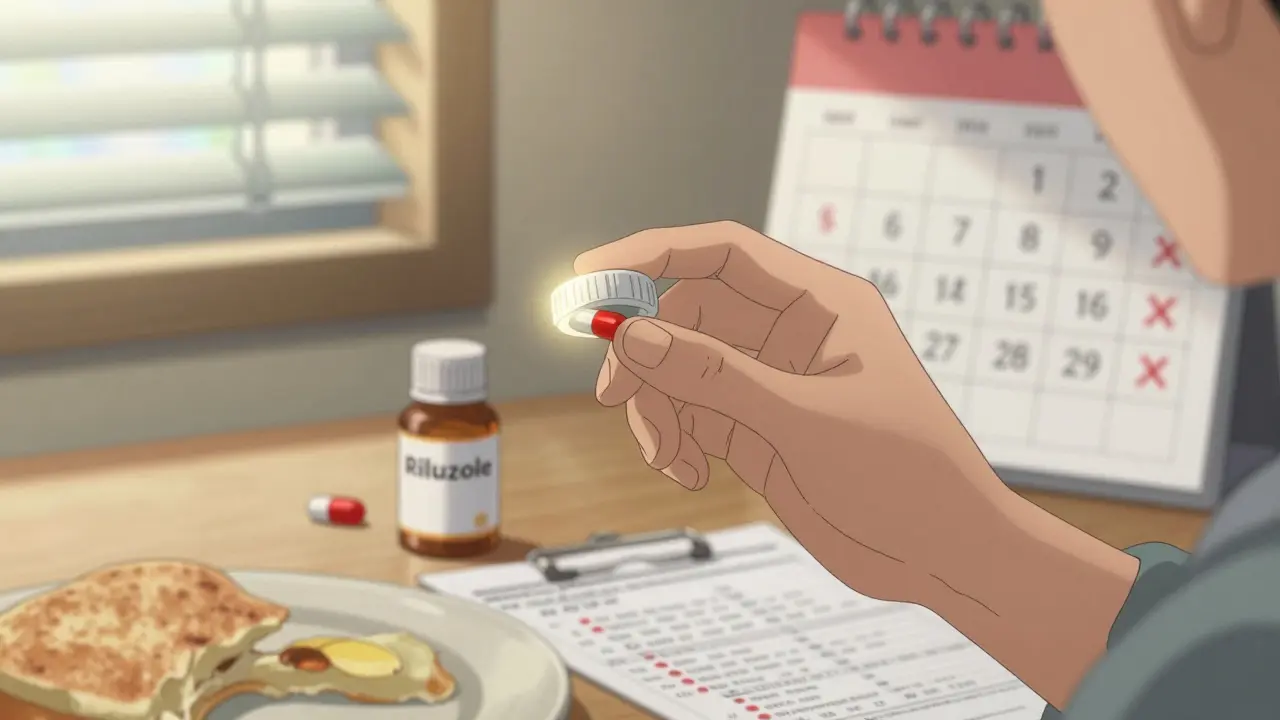
How Riluzole Is Taken - And the Cost of Taking It
Riluzole comes in three forms: tablets, liquid suspension, and an oral film that dissolves on the tongue. The standard dose is 50 mg twice a day - one in the morning, one at night. It’s not a pill you can forget. Missing doses reduces its effect. You need to take it consistently, even when you feel fine.It’s absorbed quickly - peak levels in your blood within an hour and a half. But it doesn’t stay long. Half of it leaves your system in 7 to 15 hours. That’s why twice-daily dosing is non-negotiable. If you skip a dose, don’t double up. Just take the next one on time.
But riluzole isn’t easy on the body. About 25% of people get nausea. 15% have diarrhea. Fatigue hits 1 in 5. And then there’s the liver. About 12% of users develop elevated liver enzymes - a sign of stress on the organ. That’s why doctors require blood tests before you start and every month for the first three months. If liver enzymes rise too high, you stop. No exceptions. Some patients, like one Reddit user shared, had to quit after their liver values tripled. Others, like another user, kept going because they felt their progression slowed. There’s no way to know for sure if it’s working for you - only that it might be.
Who Benefits? Who Doesn’t?
Not everyone responds the same way. In clinical trials, riluzole worked best in people with early-stage ALS - those still able to walk or speak. It showed less benefit in advanced cases. Age doesn’t seem to matter much. But weight does - lighter patients may have higher drug levels and more side effects.Real-world data tells a messier story. A 2020 review of 15 studies found that half showed clear survival benefits - up to 19 extra months in some cases. The other half saw no difference. Why the gap? Real patients are more varied than trial participants. They have other health problems. They take other meds. They don’t always stick to the schedule. And ALS itself behaves differently in each person. One person declines slowly over five years. Another loses function in months.
Still, 78% of newly diagnosed patients in the U.S. start riluzole. At one year, 63% are still on it. By two years, only 47% remain. The reasons? Side effects. Cost. Frustration. Hope. Some quit because the nausea won’t go away. Others stop because their doctor says it’s no longer useful. But many stay - not because they’re sure it’s working, but because they’re not ready to give up.
Riluzole vs. Newer Drugs
In 2017, edaravone became the second FDA-approved drug for ALS. It’s given by IV infusion and showed a 33% reduction in functional decline over six months. But it didn’t extend life. In 2023, tofersen was approved for people with a specific genetic mutation (SOD1), which affects only about 2% of ALS patients. It’s a gene-targeted therapy - expensive, complex, and only for a small group.Riluzole still holds the largest share of the ALS drug market - about 35%. It’s cheaper than edaravone or tofersen. It’s taken orally. It’s been around for nearly 30 years. Doctors still recommend it as first-line treatment. The American Academy of Neurology gives it a Level A recommendation - meaning the evidence is strong and consistent.
But here’s the truth: riluzole isn’t a breakthrough. It’s a Band-Aid on a bullet wound. It’s the only thing we’ve had for so long that we’ve learned to live with its flaws. Newer drugs are more targeted. More powerful. But they’re also more expensive, more complex, and limited to specific subtypes. For most people with ALS, riluzole is still the only option they can access.
Practical Tips for Taking Riluzole
If you’re prescribed riluzole, here’s what works:- Start with one 50 mg tablet a day for the first week. This helps your body adjust to nausea.
- Take it with food. It reduces stomach upset. Don’t take it on an empty stomach.
- Set phone alarms for morning and night. Missing doses hurts effectiveness.
- Get blood tests monthly for the first three months. Then every 3-6 months.
- Avoid caffeine-heavy drinks - coffee, energy drinks, dark tea. They can interfere with how riluzole clears from your body.
- Tell your doctor about every other medication you take. Riluzole interacts with theophylline (used for asthma) and some antidepressants.
- If you have liver disease, don’t take it. Period.
Some patients find the oral film (Exservan) easier to tolerate. It’s absorbed faster and causes fewer stomach issues. But it’s pricier and harder to get in some countries.
The Bigger Picture: Why Riluzole Still Matters
Riluzole isn’t perfect. It’s not even close. But it’s the first drug that proved ALS could be slowed - not cured, but slowed. That changed everything. Before riluzole, families were told, “There’s nothing we can do.” After riluzole, doctors could say, “There’s something.”Today, researchers are testing riluzole in combination with other drugs - like sodium phenylbutyrate - hoping to boost its effect. Early results look promising. In the future, riluzole might not be the star. But it could be part of a team - a foundation for better therapies.
For now, it remains the most widely used ALS medication worldwide. Eight in ten newly diagnosed patients take it. In wealthy countries, it’s accessible. In low-income regions, it’s out of reach for most. A single month’s supply can cost over $1,000. That’s more than many families earn in a week.
So riluzole isn’t just a drug. It’s a symbol. Of how little we know. Of how hard we’ve fought. Of how much we still need to do.
Does riluzole cure ALS?
No, riluzole does not cure ALS. It is the first drug approved to slow disease progression, modestly extending survival by an average of 2-3 months. It does not reverse damage or stop the disease, but it can delay the need for breathing support and improve the chance of living longer.
What are the most common side effects of riluzole?
The most common side effects include nausea (25%), fatigue (20%), diarrhea (15%), and elevated liver enzymes (12%). Some patients experience dizziness or weakness. Most side effects improve after the first few weeks. Liver function must be monitored monthly for the first three months of treatment.
Can you take riluzole if you have liver problems?
No. Riluzole is processed by the liver. If you have moderate to severe liver impairment (Child-Pugh Class B or C), you should not take it. The drug can build up to dangerous levels, increasing the risk of liver failure. Blood tests are required before starting and regularly during treatment.
How long does it take for riluzole to start working?
Riluzole reaches peak levels in the blood within 1-1.5 hours after taking it. But its effect on slowing disease progression isn’t immediate. Benefits are measured over months and years - not days. Patients and doctors look for slower decline in function over time, not sudden improvement.
Is riluzole effective for everyone with ALS?
No. Clinical trials show an average benefit, but real-world results vary. Some patients live significantly longer while on riluzole. Others show no measurable difference. It tends to work better in people diagnosed early, with slower-progressing forms of ALS. There’s no test to predict who will benefit.
Can you stop taking riluzole if you feel worse?
If you experience severe side effects - like jaundice, dark urine, or extreme fatigue - stop taking it and contact your doctor immediately. But if your symptoms are progressing as expected, don’t stop riluzole just because you feel worse. ALS naturally progresses, and stopping the drug won’t reverse that. Always consult your neurologist before discontinuing.
Are there alternatives to riluzole for ALS?
Yes. Edaravone (Radicava) is approved for ALS and slows functional decline, but it doesn’t extend life. Tofersen (Qalsody) is approved only for ALS caused by SOD1 gene mutations - a rare form. Riluzole remains the most widely used and accessible disease-modifying treatment for the majority of ALS patients.

