Medication Safety Assessment Tool
How to Use This Tool
Answer these simple questions to understand if you should consider an annual medication review with your pharmacist. This tool helps identify potential medication-related risks but does not replace professional medical advice.
Every year, thousands of people in Australia and around the world take medications they don’t need-or take them at the wrong time, in the wrong dose, or mixed with something that makes them dangerous. Many of these mistakes don’t show up as emergencies. They show up as fatigue, dizziness, confusion, or stomach upset. And too often, people just assume it’s part of getting older. It’s not. It could be your meds.
An annual medication review with a pharmacist isn’t just a checklist. It’s a safety reset. Think of it like a tune-up for your body’s internal system. If you’re taking four or more prescription drugs, plus vitamins, supplements, or over-the-counter painkillers, you’re at risk. Not because you’re doing anything wrong, but because the system is complicated. And pharmacists are trained to untangle it.
What Happens During an Annual Medication Review?
You walk into your local pharmacy with a bag of bottles. Not just prescriptions. Everything. That ibuprofen you take for your knees. The melatonin you use when you can’t sleep. The fish oil your sister swore by. The herbal tea you drink every night. The pharmacist sits down with you-not for five minutes, but for 30 or more. They ask: Why are you taking each one? Does it still help? Are you having any weird side effects? Have you stopped any because they made you feel worse?
This isn’t a sales pitch. It’s a deep dive. Pharmacists don’t just know what drugs do. They know how they interact. They know that mixing a blood thinner with a common painkiller can cause internal bleeding. They know that some antihistamines make seniors dizzy and increase fall risk. They know that a supplement labeled “natural” can still interfere with your heart medication.
They’ll look at your entire list and ask: Is this still necessary? Could one drug be doing the job of two? Is the dose too high for your age or kidney function? Is there a cheaper, safer alternative? Sometimes, the answer is simple: stop taking that pill. And suddenly, your headaches go away. Your stomach stops churning. Your brain feels clearer.
Why Pharmacists, Not Just Your Doctor?
Your doctor sees you for 10 minutes. They’re managing diabetes, high blood pressure, arthritis, and maybe depression. They’re not specialists in every drug on the market. But your pharmacist is. Pharmacists train for years to understand drug chemistry, interactions, side effects, and dosing across all age groups and conditions. They see hundreds of medication lists every week. They’ve seen the same mistakes repeat over and over.
And here’s the thing: most doctors don’t know what supplements you’re taking. Patients forget to mention them. Or think they’re harmless. But 40% of older adults don’t tell their doctor about their vitamins or herbal products. That’s a blind spot. A pharmacist doesn’t assume. They ask. And they write it all down.
Pharmacists also spend more time listening. If you’ve been feeling tired for months and your doctor says, “You’re just getting older,” a pharmacist might say, “Let’s look at your sleep aid and your blood pressure pill together. That combo can cause extreme fatigue.” And suddenly, you have an answer.
Who Needs This the Most?
You don’t need to be old to benefit. But if you’re 65 or older, taking five or more medications, or managing chronic conditions like heart disease, diabetes, or kidney problems-you’re in the highest-risk group. About 40% of Australians over 65 take four or more regular medications. That’s polypharmacy. And it’s the leading cause of preventable hospital admissions in older adults.
But it’s not just seniors. If you’ve been on the same meds for years and recently added something new-like an antidepressant, a steroid, or a new painkiller-you should get a review. If you’ve had a recent hospital stay, or if you’ve noticed new symptoms like confusion, memory lapses, balance issues, or nausea, those could be medication-related. Don’t wait. Book a review.
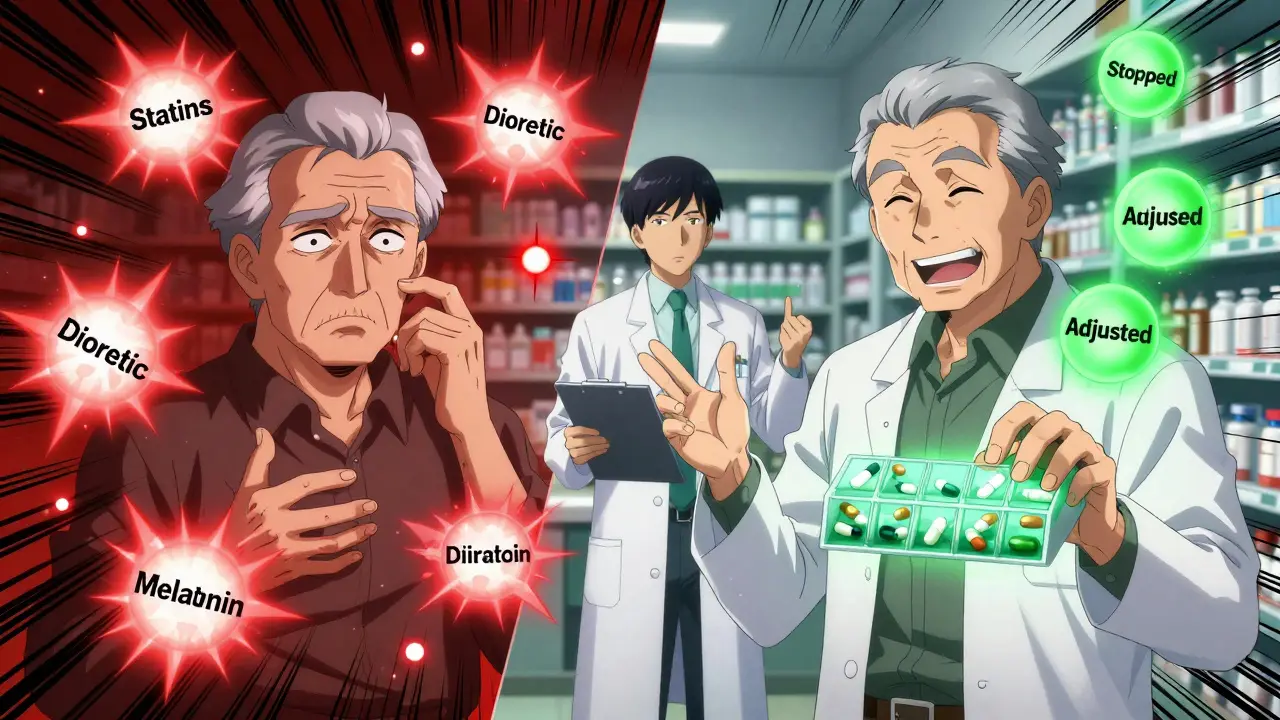
Even if you feel fine, a review can save you from future problems. One woman in Sydney came in because she was having strange leg cramps. She was on a statin for cholesterol and a diuretic for blood pressure. The pharmacist spotted the interaction. They switched her diuretic. The cramps vanished in two weeks. No one had connected the dots before.
What to Bring to Your Review
Preparation makes this quick and effective. Don’t rely on memory. Bring:
- All prescription bottles (even empty ones)
- All over-the-counter medicines (painkillers, antacids, cold meds)
- All vitamins, minerals, and supplements (including herbal teas and powders)
- A list of any recent changes-new prescriptions, stopped meds, dose changes
- Any symptoms you’ve noticed-dizziness, sleep issues, stomach upset, mood changes
If you’re overwhelmed, write it all down on paper. Use your phone’s notes app. Even a messy list is better than nothing. The pharmacist will sort it out.
What You Might Learn
Here are real things people find during their reviews:
- They’re taking two different pills for the same condition-double dosing without knowing it.
- A supplement they’ve been taking for years is interfering with their heart medication.
- A medication they stopped taking six months ago is still on their list, so their doctor keeps prescribing it.
- A side effect they thought was “just aging” is actually from a drug they started three years ago.
- They’re taking a pill at night that should be taken in the morning-and it’s wrecking their sleep.
One man in Brisbane was on seven medications. After his review, three were stopped. One was changed to a lower dose. He lost 12 pounds because his stomach wasn’t bloated anymore. He stopped feeling foggy. He said, “I didn’t know I was sick until I got better.”
How Often Should You Do This?
Once a year is the standard. But if you’ve had a big change-new diagnosis, hospital stay, new doctor, or new meds-don’t wait. Get a review then. If you’re on high-risk meds like blood thinners, opioids, or diabetes drugs, twice a year might be better.
Some pharmacies offer automated reminders. Ask if yours does. Medicare and some private insurers cover this service. In Australia, it’s often free through community pharmacies under the Chronic Disease Management plan or Pharmaceutical Benefits Scheme. You don’t need a referral. Just walk in.
What If Your Pharmacist Says You Don’t Need It?
That’s rare. But if they say you’re on just one or two simple meds and have no side effects, they might be right. Still, ask: “Can you check for interactions with anything I might start in the future?” Or, “If I start a new medication next month, should I come back?”
Don’t let them dismiss you. You know your body. If you feel off, it’s worth a second look. And if your pharmacist doesn’t take it seriously, find another one. Not all pharmacies offer the same level of care. Look for pharmacies with a Medication Therapy Management (MTM) program. Ask if they have a pharmacist trained in geriatric or chronic disease management.
What Happens After the Review?
At the end, you’ll get a written summary. It will list:
- What you’re currently taking
- What was changed, stopped, or added
- Why each change was made
- What side effects to watch for
- When to follow up
The pharmacist will also send a copy to your doctor-with your permission. That’s critical. A review is only as good as the follow-up. If your doctor doesn’t know about the changes, they might prescribe something that conflicts with the new plan.
Some pharmacies offer free blister packs or pill organizers to help you stay on track. Others will sync your refills so you don’t run out of one pill while others pile up. These small tools make a huge difference in adherence-and safety.
Why This Matters More Than Ever
By 2030, one in four Australians will be over 65. More people are living with multiple chronic conditions. More drugs are being prescribed. More people are self-medicating with supplements. The risk of harm is rising. But the solution is simple, safe, and accessible.
Pharmacists are the most underused resource in healthcare. They’re not doctors. They’re not nurses. They’re medication experts. And they’re right down the street.
Every year, around 1.5 million adverse drug events happen in the U.S. alone. Many are preventable. In Australia, medication errors contribute to over 20% of hospital admissions in older adults. That’s not bad luck. That’s a system failure. And an annual review is the fix.
You don’t need to wait for a crisis. You don’t need to be sick. You just need to be smart. Take an hour once a year. Bring your meds. Ask the questions. Let someone who knows drugs inside out help you cut through the noise. You might not feel a difference right away. But next year, when you’re still feeling strong, clear-headed, and safe-you’ll know why.