Anticholinergic Side Effect Risk Calculator
Your Risk Assessment
Why This Matters
First-generation antihistamines (like diphenhydramine) block acetylcholine, causing dry mouth, constipation, and urinary issues. Long-term use increases dementia risk by 54%.
Your Personalized Risk Report
First-Generation Antihistamines
High RiskFor people over 65 with symptoms
Second-Generation Antihistamines
Low RiskMinimal anticholinergic effects
Recommended Actions
- Switch to second-generation antihistamines like cetirizine, loratadine, or fexofenadine
- Check medication labels for diphenhydramine
- Consider safer alternatives if over 65 or with prostate issues
When you reach for a bottle of Benadryl for your allergies, you’re probably thinking about stopping the sneezing and itchy eyes. But what you might not realize is that you’re also hitting a hidden switch in your body-one that shuts down important functions like saliva production, bowel movement, and bladder control. This isn’t a side effect you can ignore. It’s a direct result of something called anticholinergic effects, and it’s happening in millions of people every day, especially those over 65.
What Exactly Are Anticholinergic Effects?
Anticholinergic effects happen when a drug blocks acetylcholine, a chemical your body uses to send signals between nerves and organs. Think of it like cutting the wires to your body’s internal controls. Histamine blockers-antihistamines-are supposed to stop allergy symptoms by blocking histamine. But first-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine don’t stop there. They also bind tightly to muscarinic receptors, which control things like saliva, digestion, and urination. This isn’t a flaw in the drug-it’s built in. These drugs were designed in the 1940s, before scientists fully understood how specific receptors work. They were made from compounds already known to dry things out, because back then, sedation was seen as a bonus, not a risk.Dry Mouth: More Than Just an Inconvenience
You’ve probably noticed it: that thick, sticky feeling in your mouth after taking diphenhydramine. That’s not dehydration. That’s your salivary glands being shut down. Studies show first-generation antihistamines can reduce saliva flow by 60-70%. This isn’t just uncomfortable-it’s dangerous. Dry mouth leads to tooth decay, gum disease, and mouth infections. The American Dental Association says chewing sugar-free gum with xylitol can boost saliva by 40-60% within minutes. But if you’re taking these meds daily, that’s a band-aid on a broken pipe. Long-term dry mouth increases your risk of cavities by 3-5 times, according to dental research from 2022. And most people don’t even realize it’s the medication causing it. A 2020 study found only 28% of patients could correctly link dry mouth to their antihistamine use.Constipation: The Silent Side Effect
Your gut runs on acetylcholine. It tells your intestines to contract and move things along. When antihistamines block those signals, your digestion slows down. First-generation antihistamines can increase bowel transit time by 1.5 to 2 times normal. That means food sits longer, water gets sucked out, and stool hardens. About 15-20% of users report constipation. For older adults, especially those with existing bowel issues, this can lead to fecal impaction-a medical emergency. The American Gastroenterological Association recommends taking polyethylene glycol (17g daily) as a preventive measure if you must use these drugs. In one trial, this cut constipation rates from 18% to just 5%. But again, most people don’t know to ask for it. They just think, “I’m not eating enough fiber,” and keep taking the pill.Urinary Retention: A Real Danger for Men
For men with enlarged prostates, this is where things get serious. First-generation antihistamines tighten the urethral sphincter and weaken the bladder’s ability to contract. The result? Incomplete emptying-or worse, total urinary retention. Studies show 5-8% of older men on these drugs develop acute urinary retention within 48 hours. That means you can’t pee at all. It’s painful. It requires a catheter. And it’s preventable. The American Urological Association says men with an International Prostate Symptom Score above 8 should avoid these drugs entirely. Yet, many doctors still prescribe them. A 2023 survey found that 31% of men with moderate to severe prostate symptoms were still using diphenhydramine for allergies. They didn’t know the risk. Their pharmacist didn’t warn them. And their doctor didn’t ask.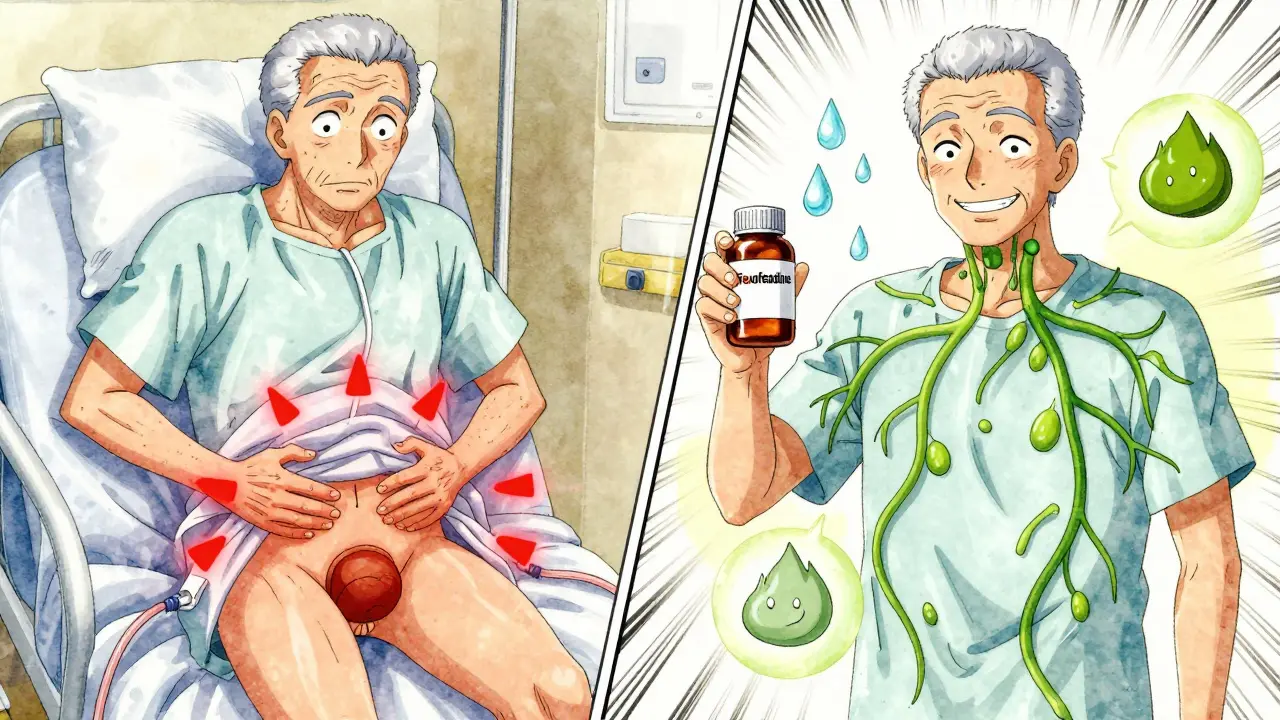
First-Gen vs. Second-Gen: The Clear Difference
Not all antihistamines are the same. Second-generation drugs like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were made to avoid these problems. They barely touch muscarinic receptors. Here’s what the data shows:| Side Effect | First-Generation (e.g., Diphenhydramine) | Second-Generation (e.g., Cetirizine, Fexofenadine) |
|---|---|---|
| Dry Mouth | 28% | 2-4% |
| Constipation | 15-20% | 3-5% |
| Urinary Retention (in elderly men) | 5-8% | <1% |
| Duration of Action | 4-6 hours | 24 hours |
| Typical Dose | 25-50 mg | 10 mg |
Second-gen antihistamines work just as well for allergies-with none of the collateral damage. And they last longer. One dose a day. No need to re-dose every 4-6 hours. You’re not just avoiding dry mouth-you’re avoiding the daily hassle of managing side effects.
Why Do People Still Use First-Generation Antihistamines?
Price and availability. Generic diphenhydramine costs $4-6 for 24 doses. Loratadine or fexofenadine? $12-18. That’s a big difference for people on tight budgets. They’re also in many multi-symptom cold and sleep aids. If you’re buying something labeled “Nighttime Allergy Relief,” you’re probably getting diphenhydramine-even if you didn’t realize it. And because it makes you sleepy, many people use it as a sleep aid. But here’s the catch: the sedation isn’t clean. It’s foggy, groggy, and lingering. That’s not rest-it’s chemical impairment.The Cognitive Risk: More Than Just a Dry Mouth
The biggest concern isn’t just constipation or trouble peeing. It’s your brain. Long-term use of first-generation antihistamines is linked to a 54% higher risk of dementia over seven years, according to a landmark 2015 study in JAMA Internal Medicine. Each year of use beyond 90 daily doses adds another 20% risk. That’s not a small number. The American Geriatrics Society lists these drugs as “potentially inappropriate” for older adults. The European Academy of Allergy and Clinical Immunology says to avoid them entirely in patients over 65. And Mayo Clinic stopped using diphenhydramine in its hospitals in 2022 because of too many cases of anticholinergic delirium-patients suddenly confused, disoriented, and hallucinating after just a few doses.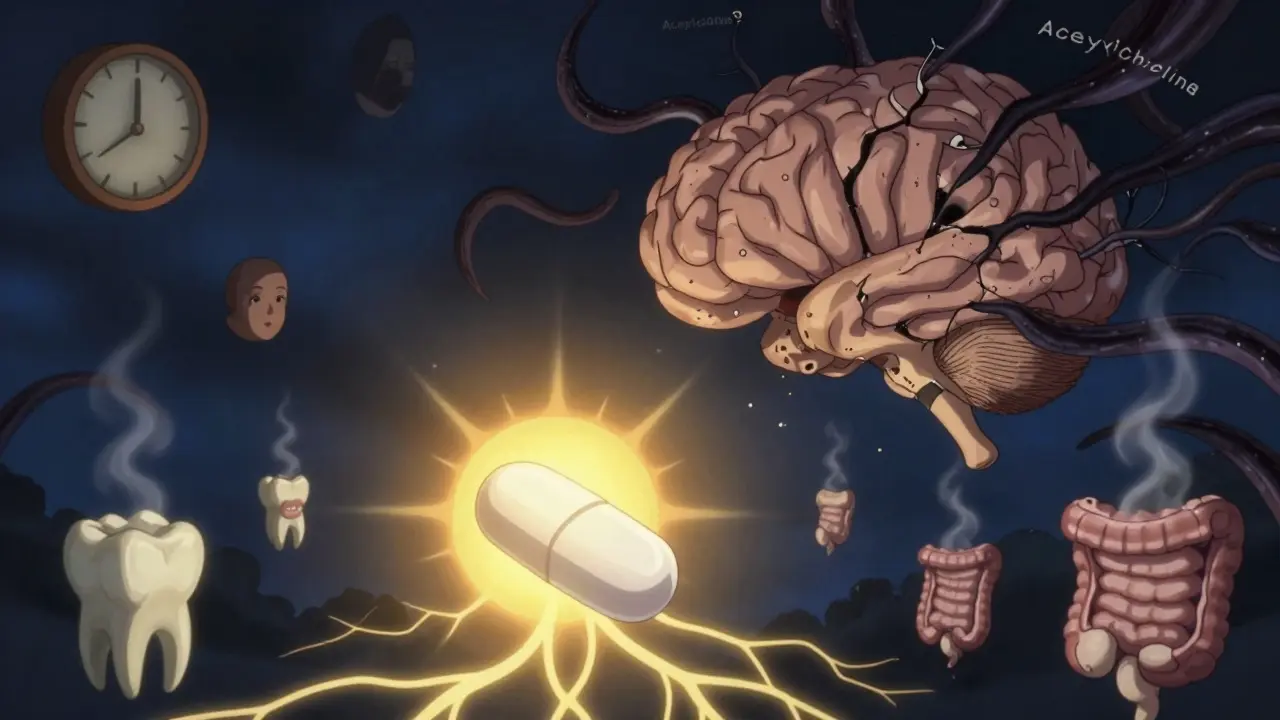
What Should You Do?
If you’re taking diphenhydramine, chlorpheniramine, or promethazine regularly for allergies or sleep:- Switch to a second-generation antihistamine: cetirizine, loratadine, or fexofenadine. They’re just as effective, safer, and last longer.
- Check your cold and sleep meds. Many contain diphenhydramine under “active ingredients.” Look for “diphenhydramine HCl” or “pheniramine.”
- If you’re over 65 or have prostate issues, constipation, or glaucoma, talk to your doctor about stopping these drugs entirely.
- Don’t use them as sleep aids. The risks far outweigh the benefits. Try melatonin or behavioral sleep strategies instead.
- If you’ve had dry mouth or urinary issues and didn’t know why, ask your pharmacist to review all your medications. You might be surprised.
What’s Next?
New antihistamines are coming. In 2023, the FDA approved olopatadine nasal spray-no anticholinergic activity at all. Researchers are now testing H4 receptor blockers that target allergies without touching any other receptors. The Alzheimer’s Association is funding a $2.5 million study to track whether switching from first- to second-generation antihistamines slows cognitive decline in older adults. Results aren’t due until 2026. But the trend is clear: the era of first-generation antihistamines is ending. Not because they don’t work. But because we now know how much they cost.Are all antihistamines the same when it comes to side effects?
No. First-generation antihistamines like diphenhydramine and chlorpheniramine have strong anticholinergic effects, causing dry mouth, constipation, and urinary retention. Second-generation antihistamines like cetirizine, loratadine, and fexofenadine were designed to avoid these effects and rarely cause them at standard doses.
Can antihistamines cause dementia?
Long-term use of first-generation antihistamines is linked to a 54% increased risk of dementia over seven years, according to research published in JAMA Internal Medicine. The risk rises with each year of use, especially in people over 65. This is why experts now advise avoiding these drugs in older adults.
Why is dry mouth from antihistamines dangerous?
Dry mouth reduces saliva, which normally protects teeth from decay and neutralizes acids. Chronic dry mouth increases the risk of cavities, gum disease, and oral infections. It can also make chewing and swallowing difficult, leading to poor nutrition. The American Dental Association recommends sugar-free gum with xylitol to help stimulate saliva flow.
Should men with enlarged prostates avoid antihistamines?
Yes. First-generation antihistamines can cause acute urinary retention in men with enlarged prostates. Studies show 31% of men with moderate to severe symptoms experience this within 48 hours of taking diphenhydramine. The American Urological Association advises avoiding these drugs entirely in this group.
Is it safe to use diphenhydramine as a sleep aid?
No. While diphenhydramine makes you drowsy, it causes poor-quality sleep, next-day grogginess, and increases fall risk by 34% in older adults. It also carries long-term cognitive risks. Safer alternatives include melatonin, cognitive behavioral therapy for insomnia (CBT-I), or improving sleep hygiene.
What are the best alternatives to first-generation antihistamines?
Cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are equally effective for allergies with minimal side effects. Olopatadine nasal spray is another option with no anticholinergic activity. All are available over-the-counter and are safe for daily use in most adults, including older patients.

