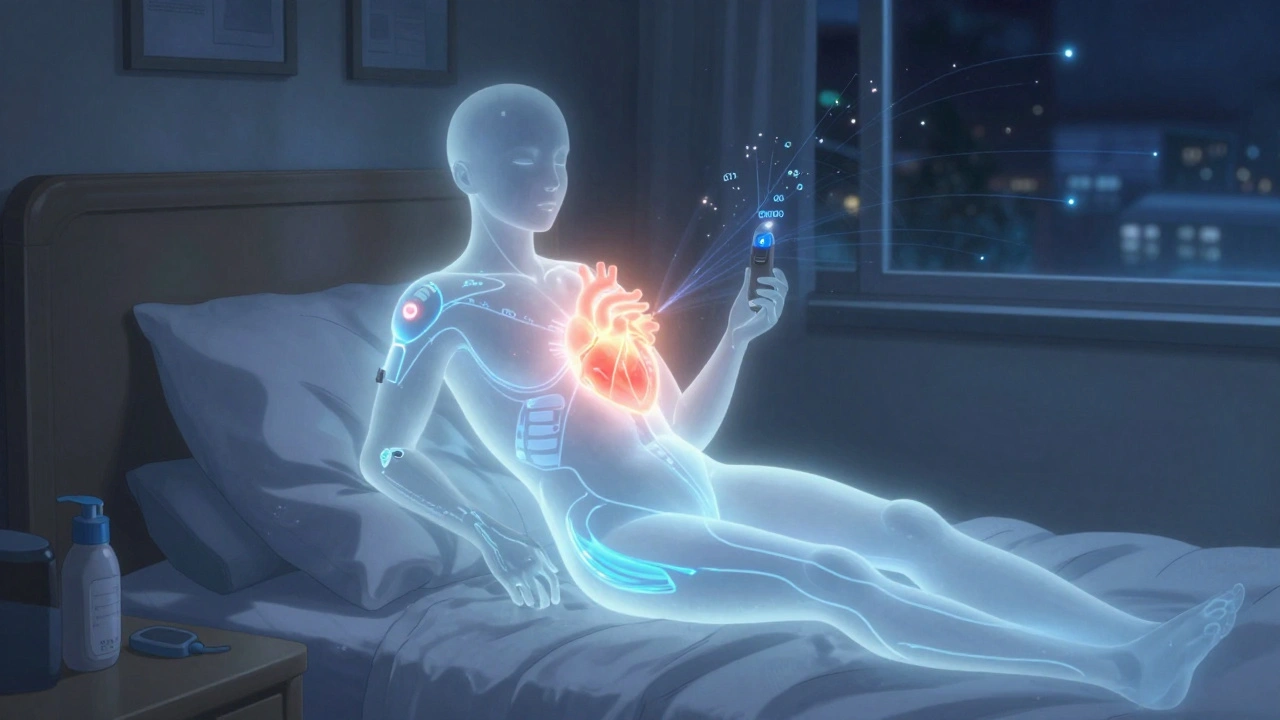
When you have type 1 diabetes, your body doesn’t make insulin. That means you have to replace it-every single day. But not just any insulin plan will do. If you want real control over your blood sugar-not just avoiding highs and lows, but living without constant fear-you need a system that works like your pancreas used to. That’s where basal-bolus insulin comes in.
What Basal-Bolus Insulin Actually Does
Basal-bolus insulin isn’t one shot. It’s two kinds of insulin working together. Basal insulin is your background dose. It’s long-acting, steady, and keeps your blood sugar from creeping up overnight or between meals. Think of it like a slow drip of insulin that never stops. Bolus insulin is your mealtime dose. It’s fast-acting, peaks quickly, and covers the carbs you eat or corrects a high reading. This isn’t just theory. Back in 1993, the Diabetes Control and Complications Trial proved that people with type 1 diabetes who used this kind of intensive insulin therapy cut their risk of eye, kidney, and nerve damage by up to 76%. That’s why today, every major guideline-from the American Diabetes Association to the European Association for the Study of Diabetes-says basal-bolus is the gold standard for type 1 diabetes. But here’s the thing: it’s not just for type 1. If you have type 2 diabetes and your pills and basal insulin alone aren’t cutting it, adding bolus doses can drop your A1c by another 1% to 1.5%. That’s the difference between a risky 8.5% and a much safer 7%.How to Calculate Your Total Daily Dose
The first step in starting basal-bolus isn’t picking a brand of insulin. It’s figuring out how much you need total. Most people start with 0.5 units of insulin per kilogram of body weight. So if you weigh 70 kg (about 154 pounds), your starting total daily dose is around 35 units. Some clinics use a simpler trick: divide your weight in pounds by 4. A 160-pound person gets 40 units total. That total gets split two ways. About half goes to basal, half to bolus. That’s the 50/50 rule. For our 160-pound person (40 units total), that means 20 units of basal insulin and 20 units of bolus insulin. Basal insulin is usually taken once a day-sometimes twice, depending on the type. Common choices are glargine (Lantus, Basaglar), detemir (Levemir), or degludec (Tresiba). These last 20 to 40 hours and don’t have a strong peak. That’s good. You want smooth, steady coverage.Starting Your Bolus Dose
Now for the bolus. That’s the part people struggle with the most. You don’t just inject the same amount every meal. You adjust based on what you’re eating and what your blood sugar is right now. Start with 4 units per day total for bolus, or 10% of your basal dose. So if your basal is 20 units, start with 2 units per meal. That’s your baseline. Then you learn two key numbers: your carb ratio and your correction factor. Your carb ratio tells you how much one unit of insulin covers. Use the 500 Rule: divide 500 by your total daily insulin. If you’re on 40 units total, 500 ÷ 40 = 12.5. That means one unit of insulin covers about 12.5 grams of carbs. So if you eat a sandwich with 50 grams of carbs, you’d need about 4 units of insulin (50 ÷ 12.5). Your correction factor tells you how much one unit lowers your blood sugar. Use the 1700 Rule: divide 1700 by your total daily insulin. For 40 units, that’s 42.5. So one unit drops your blood sugar by about 42 mg/dL. If your reading is 200 and your target is 120, you’re 80 points high. 80 ÷ 42.5 = 1.9 units. Round to 2 units. Add those together: carb dose + correction dose = your total bolus.
Why This Works Better Than Other Plans
Some people use premixed insulin-like 70/30-which combines long- and short-acting in one shot. It’s simpler. But it’s also rigid. You have to eat at the same time, every day. No flexibility. No room for a late lunch or a surprise dessert. Basal-bolus gives you freedom. You can skip a meal. You can eat pizza on Saturday. You can go for a run after dinner. You just adjust your bolus. Studies show people on basal-bolus have lower A1c levels than those on premixed insulin-by about 0.4%. But here’s the trade-off: you get more low blood sugar episodes. About 1.3 times more. That’s why education matters. A 2022 survey found that 42% of new users needed extra training after their initial class. You can’t just hand someone a prescription and expect them to figure out carb counting on their own.Who It’s For-and Who Should Avoid It
Basal-bolus is ideal for:- People with type 1 diabetes (it’s the standard)
- Those with type 2 who still have high blood sugar after meals
- People who eat irregularly or have unpredictable schedules
- Those who want to get their A1c below 7%
- People with cognitive issues or memory problems
- Those with limited hand dexterity who can’t handle multiple injections
- Patients who refuse to count carbs or check blood sugar often
- Older adults over 65-only 35% use it, compared to 82% under 45
The Real-Life Challenges
I’ve talked to people who’ve been on basal-bolus for years. One user on Reddit said: “I’ve been doing this for two years and I still second-guess my doses before every meal.” That’s normal. The biggest hurdles:- Carb counting accuracy-most people are off by 10-15 grams
- Timing insulin too early or too late
- Not adjusting for exercise
- Fear of low blood sugar