When you're breastfeeding, taking a pill for a headache, an infection, or even depression can feel risky. You wonder: Will this medicine hurt my baby? The truth is, most medications are safe. But not all. And knowing which ones are okay - and which ones need caution - isn't just helpful, it's essential.
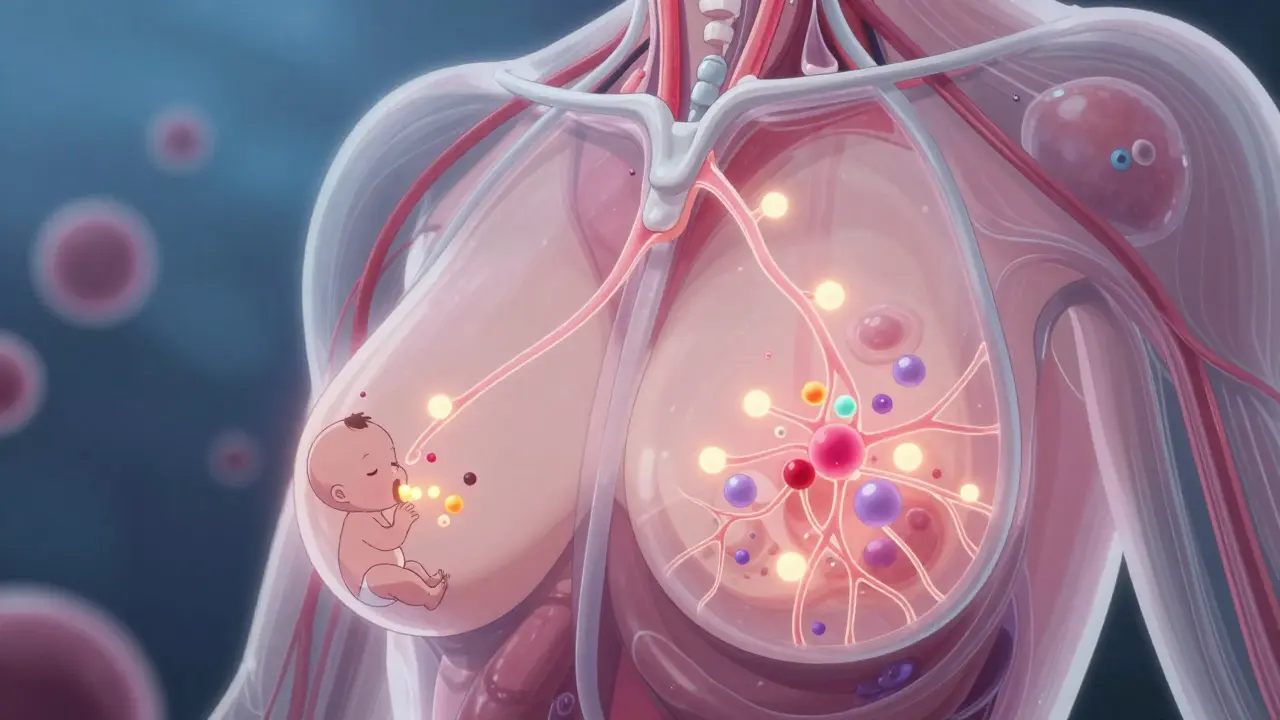
How Medications Get Into Breast Milk
Medications don’t magically appear in breast milk. They travel from your bloodstream into your milk through a natural process called passive diffusion. Think of it like water seeping through a sponge. The drug moves from where it’s more concentrated (your blood) to where it’s less concentrated (your milk). But not every drug does this the same way. Four main factors decide how much ends up in your milk:- Molecular weight: Smaller molecules (under 200 daltons) slip through easily. Most common drugs fall into this range.
- Lipid solubility: Fats help drugs cross cell membranes. The more fat-soluble a drug is, the more likely it is to enter milk.
- Protein binding: If a drug sticks tightly to proteins in your blood (over 90%), it can’t easily leave your bloodstream to reach your milk.
- Half-life: Drugs that stay in your system longer (over 24 hours) have more time to build up in milk. Shorter half-life drugs clear faster.
There’s also something called ion trapping. Your blood is slightly more alkaline (pH 7.4) than breast milk (pH 7.2). Weakly basic drugs - like certain antidepressants or pain relievers - can get trapped in milk, leading to higher concentrations. That’s why lithium, for example, needs careful monitoring.
Early on, right after birth, your milk is colostrum. It’s thick, sticky, and made in tiny amounts - just 30 to 60 milliliters a day. The gaps between the cells in your breasts are wider then, so drugs can move in more easily. But because your baby drinks so little, their total exposure is still low. By day five to seven, your milk volume increases dramatically, but the cell barriers tighten up, reducing how much drug gets through.
How Much of the Drug Actually Reaches Your Baby?
Most mothers assume if a drug is in their milk, their baby is getting a strong dose. That’s not true. Even when a drug shows up in breast milk, the amount your baby actually swallows is tiny. On average, infants receive less than 1% of the mother’s weight-adjusted dose. For most medications, that’s far below what would be prescribed to a newborn. In fact, the CDC reports that fewer than 2% of breastfed infants experience any clinically significant side effects from medication exposure. Why? Because babies don’t absorb everything they swallow. Their digestive systems are still developing. Many drugs - especially those that are poorly absorbed in the gut - pass right through without ever entering the baby’s bloodstream. That’s why drugs like certain antibiotics or antihistamines are considered safe, even when they show up in milk.The L1 to L5 Risk System - What You Need to Know
Dr. Thomas Hale, a leading expert in lactation pharmacology, created the most trusted classification system for medications during breastfeeding. It’s simple: five categories, from safest to most dangerous.- L1 (Safest): No documented risk. Examples: acetaminophen, ibuprofen, penicillin.
- L2 (Safer): Limited data, but no adverse effects reported. Examples: sertraline, ciprofloxacin, albuterol.
- L3 (Moderately Safe): Risk can’t be ruled out. Use with caution. Examples: fluoxetine, amitriptyline, metformin.
- L4 (Possibly Hazardous): Evidence of risk exists. Use only if benefits outweigh risks. Examples: lithium, cyclosporine.
- L5 (Contraindicated): Proven risk. Avoid completely. Examples: radioactive isotopes, chemotherapy drugs, ergotamine.
This system is used by doctors, pharmacists, and lactation consultants worldwide. It’s not perfect - but it’s the best tool we have. And here’s the key: only about 1% of medications are L4 or L5. That means for nearly every drug you’re prescribed, you can keep breastfeeding.
Top Medications Used While Breastfeeding - And What the Data Says
Most women take medications while breastfeeding. A 2022 study found that over half of nursing mothers use at least one drug. The most common are:- Analgesics (28.7%): Acetaminophen and ibuprofen are top choices. Both have minimal transfer and no reported harm. Avoid aspirin and codeine - they can cause rare but serious reactions in babies.
- Antibiotics (22.3%): Penicillins, cephalosporins, and clindamycin are safe. Even metronidazole, once thought risky, is now considered compatible when used in short courses.
- Psychotropics (15.6%): Sertraline is the go-to antidepressant. It has the lowest transfer rate and the most safety data. Fluoxetine and paroxetine are also options, but sertraline remains the gold standard.
For thyroid meds like levothyroxine, you can continue breastfeeding - the drug doesn’t transfer in meaningful amounts. Birth control pills? Progestin-only pills are fine. Estrogen-containing pills can reduce milk supply, so they’re usually avoided in early breastfeeding.
What about herbs and supplements? LactMed now includes over 350 herbal products and 200 dietary supplements. But here’s the catch: many aren’t tested. St. John’s Wort, for example, may cause irritability or colic in infants. Turmeric? Probably safe. But don’t assume “natural” means “safe.” Always check.
When and How to Take Medications to Minimize Risk
Timing matters. You don’t have to stop breastfeeding - you just need to be smart about when you take your pills.- Take meds right after breastfeeding: This gives your body time to clear the drug before the next feeding. If you take a pill at bedtime, your baby sleeps through the peak concentration.
- Use short-acting drugs: Choose medications with a half-life under 4 hours when possible. That way, levels drop quickly.
- Avoid extended-release forms: These keep drug levels high for longer, increasing exposure.
- Use topical treatments when you can: Creams and patches (like lidocaine or nicotine patches) deliver less to milk than pills. Just avoid applying them directly to the nipple.
For drugs taken multiple times a day, time them right after each feeding. For once-daily meds, take them after the longest stretch of sleep - usually after the night feeding.
Where to Find Reliable Information - And What to Avoid
Not all sources are created equal. Google “is this safe while breastfeeding?” and you’ll get conflicting answers. Here’s what to trust:- LactMed: Run by the U.S. National Library of Medicine. Free. Updated daily. Covers over 4,000 drugs, 350 herbs, and 200 supplements. Used by 1.2 million people a year. It’s technical, but accurate.
- Hale’s Medications and Mothers’ Milk: The go-to clinical guide. Uses the L1-L5 system. More user-friendly than LactMed. Great for quick decisions.
- MotherToBaby: A free service by OTIS. Call or chat with specialists. They handle about 15,000 calls a year. No charge. No sales pitch.
Avoid: Pinterest posts, Facebook groups, or well-meaning relatives who say, “I heard this is bad.” If it’s not from LactMed, Hale, or a healthcare provider who checks these sources, don’t rely on it.
What to Watch For in Your Baby
Most babies show no reaction. But if you notice any of these, talk to your doctor:- Unusual sleepiness or fussiness
- Changes in feeding patterns
- Diarrhea or vomiting
- Rash or hives
- Jaundice that doesn’t improve
These are rare. But if they happen, don’t panic. Most reactions are mild and go away when you stop the drug. Your doctor can help you switch to a safer option - without stopping breastfeeding.
The Bigger Picture: Why This Matters
A 2021 survey of 500 lactation consultants found that 78% saw at least one mother per month who was wrongly told to stop breastfeeding because of a medication. That’s heartbreaking. And unnecessary. Breastfeeding lowers your baby’s risk of infections, allergies, obesity, and sudden infant death syndrome. For you, it reduces risks of breast cancer, ovarian cancer, and type 2 diabetes. Giving up breastfeeding over a medication that’s actually safe means losing all that - for no good reason. New research is coming fast. The FDA now encourages drug makers to include nursing women in trials. By 2030, doctors may use genetic testing to predict exactly how much of a drug will end up in your milk - making recommendations even more precise.Bottom Line: You Can Breastfeed - Even With Medications
You don’t have to choose between being healthy and feeding your baby. Most medications are safe. The risk of harm from the drug is far lower than the risk of stopping breastfeeding. Talk to your doctor. Use LactMed or Hale’s guide. Time your doses wisely. Watch your baby. And remember: if your doctor says to stop breastfeeding, ask them to check LactMed first. You’re not being difficult - you’re being informed.Medication and breastfeeding aren’t enemies. They can work together - if you know how.

