Every year, millions of people are diagnosed with cancer. But here’s the truth: cancer prevention isn’t just for doctors and researchers. It’s something you can act on today-with real, measurable results. The World Health Organization says 30-40% of all cancers are preventable. That’s not a guess. It’s based on decades of data from over 11,000 studies. You don’t need a miracle drug or a radical surgery. You need to change how you live.
What Lifestyle Changes Actually Lower Cancer Risk?
It’s not about perfection. It’s about consistency. The American Cancer Society’s updated 2020 guidelines lay out clear, science-backed steps. And the numbers don’t lie. If you stick to just three of them-staying active, eating more plants, and keeping your weight in check-you can cut your cancer risk by 18-21% in five years. That’s not theoretical. It’s what Harvard’s T.H. Chan School of Public Health found in tracking over 100,000 people.
Let’s break it down. First, move more. You don’t need to run marathons. Aim for 150 minutes a week of brisk walking-that’s 30 minutes, five days a week. Studies show this alone lowers colon cancer risk by 24% and breast cancer by 12-20%. Why? Movement reduces inflammation, balances hormones, and helps your immune system spot abnormal cells early.
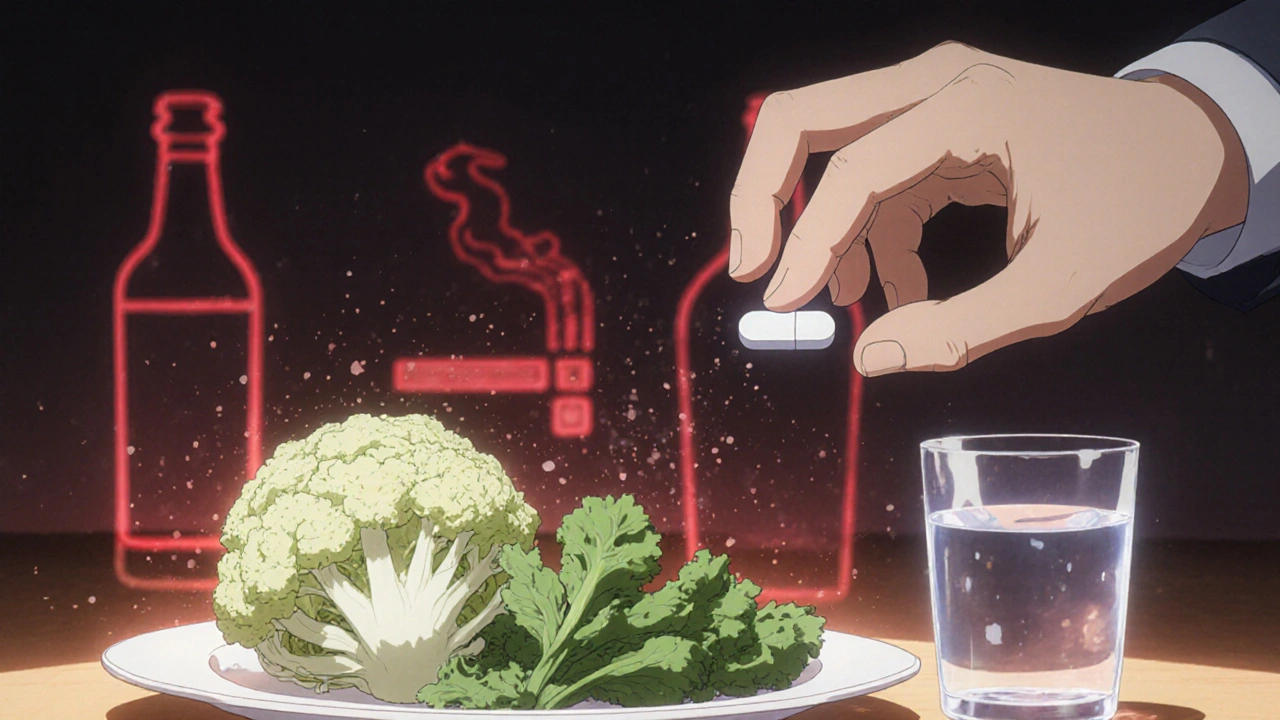
Next, eat more vegetables and fruits. Not just a side salad. Think 2.5 to 3 cups of veggies and 1.5 to 2 cups of fruit daily. Cruciferous veggies like broccoli, cauliflower, and kale have been linked to up to 20% lower prostate cancer risk. Why? They contain compounds like sulforaphane that help turn off cancer-promoting genes. And don’t skip the fruit. Berries, citrus, and apples are packed with antioxidants that protect your cells from damage.
Weight matters. Every 5-point increase in BMI above 25 raises your risk of postmenopausal breast cancer by 12%, kidney cancer by 10%, and colorectal cancer by 8%. You don’t need to lose 50 pounds. Even a 5-10% drop in body weight-say, 10-15 pounds for someone who weighs 150-can reduce tumor-promoting inflammation by 25-30% within six months, according to research from the University of Arizona.
Tobacco and Alcohol: The Two Biggest Avoidable Risks
If you smoke, quitting is the single most powerful thing you can do to prevent cancer. Cancer Research UK reports smoking causes 78% of lung cancers and 15-20% of all cancer deaths. It doesn’t matter if you’ve smoked for 20 years. Your body starts repairing itself within hours. After five years, your risk of mouth, throat, and esophageal cancers drops by half. After 10 years, lung cancer risk is cut in half compared to someone still smoking.
Alcohol is the other big one. Most people think a glass of wine is harmless. But here’s the data: each extra drink per day increases breast cancer risk by 7-12%. For esophageal cancer, it’s 20-30% higher with just one daily drink. The guidelines are simple: men, no more than two standard drinks a day (28g ethanol). Women, no more than one (14g). That’s one 12-oz beer, one 5-oz glass of wine, or one 1.5-oz shot of spirits. And no, red wine isn’t a magic shield. The alcohol is the problem.
Food Choices That Help-and Harm
Not all processed foods are equal. The World Cancer Research Fund and American Institute for Cancer Research classify processed meats-like bacon, sausage, hot dogs, and deli meats-as Group 1 carcinogens. That’s the same category as tobacco. Eating just 50 grams a day (about two slices of bacon) raises colorectal cancer risk by 18%. The WCRF/AICR recommends avoiding them entirely. The American Cancer Society says you can have up to 18 ounces a week, but that’s the limit, not a target.
What should you eat instead? Focus on whole, unprocessed foods. Beans, lentils, whole grains, nuts, seeds, and fish are all linked to lower cancer rates. A 2024 meta-analysis from UC Davis Health found people who ate legumes at least four times a week had 15% lower risk of colorectal cancer. Fiber doesn’t just help digestion-it feeds your gut bacteria, which in turn help regulate immune responses that can suppress tumor growth.
And sugar? It’s not a direct cause, but it fuels obesity. And obesity fuels cancer. Cutting back on sugary drinks and snacks isn’t about willpower-it’s about reducing insulin spikes. High insulin levels promote cell growth, including cancerous ones.
Sun Exposure and Skin Cancer: Simple Rules, Big Impact
Most people know the sun causes skin cancer. But how many know the exact numbers? Mayo Clinic’s 2022 review found that using SPF 30+ broad-spectrum sunscreen every day, reapplying every two hours, cuts melanoma risk by 50%. And it’s not just beach days. Daily exposure-even walking to your car or sitting by a window-adds up. UV radiation peaks between 10 a.m. and 4 p.m., when 80% of daily exposure happens. Wear a wide-brimmed hat, sunglasses, and seek shade during those hours. Skin cancer is one of the most preventable cancers, but only if you treat sun protection like brushing your teeth: non-negotiable, daily.
What Is Chemoprevention? And Does It Work?
Chemoprevention sounds like a drug, and it is-but it’s not for everyone. It means using natural or synthetic substances to stop cancer before it starts. The most proven examples are aspirin and tamoxifen.
Low-dose aspirin (75-100mg daily) has been shown in multiple trials to reduce colorectal cancer risk by 20-40% over 10 years. But it’s not for everyone. It can cause stomach bleeding or ulcers. Only people with a high risk-like those with Lynch syndrome or a strong family history-should consider it, and only under a doctor’s supervision.
Tamoxifen and raloxifene reduce breast cancer risk by 30-50% in high-risk women. But again, side effects like blood clots and hot flashes mean they’re only recommended for those with a 3% or higher 5-year risk, based on tools like the Gail Model. These aren’t magic pills. They’re targeted tools for specific cases.
For most people, chemoprevention isn’t the first step. Lifestyle is. Chemoprevention is the backup plan for those who need extra protection.
Why Most People Struggle-And How to Succeed Anyway
UCLA’s 2023 survey of 1,200 people found 68% struggle to stay active. Why? Time. 74% said they just don’t have enough of it. And 52% say they can’t eat enough veggies. The problem isn’t willpower. It’s systems.
Successful programs don’t ask for big changes. They start small. UC Davis Health’s ‘Cultivating Health’ program pairs activity tracking with group support. Participants hit 85% of their weekly goals-not because they’re super disciplined, but because they had accountability. The American Cancer Society’s ‘3-2-1’ rule works because it’s simple: 30 minutes of movement daily, 2 servings of vegetables at lunch or dinner, and 1 hour less screen time. That’s it.
And here’s the secret: focus on one change at a time. A 2023 ACS report showed 78% of people kept up a single habit after 12 months. But only 32% stuck with three changes. Start with walking. Then add a veggie to dinner. Then cut out sugary drinks. Slow wins the race.
The Bigger Picture: Who’s Getting Help-and Who’s Not
The cancer prevention market is worth $186.7 billion. But the benefits aren’t evenly shared. Only 29% of Medicaid patients get lifestyle counseling from their doctors. That’s compared to 67% of privately insured patients. Hispanic adults and people in the Southern U.S. are the least likely to meet vegetable intake goals. Only 12% of U.S. adults eat enough veggies. And only 31% get enough exercise.
Public awareness is also uneven. 64% know smoking causes cancer. Only 28% know obesity does. That’s why education matters. The NIH’s 2024-2028 plan is investing $287 million into digital tools-apps, wearables, AI coaching-to make prevention easier. ASCO is training 5,000 oncologists to talk about lifestyle by 2025. But until your doctor asks you about your diet or activity level, you have to ask first.
What’s Next? Personalized Prevention Is Coming
The future isn’t one-size-fits-all. The NCI-MATCH trial is testing whether your genes can guide your diet. If you have a certain mutation, maybe you need more cruciferous veggies. If you have another, maybe you need more omega-3s. Preliminary results are expected in late 2025.
Harvard’s $15 million study tracking 120,000 people will finally answer the big question: do combined lifestyle changes have a bigger effect than the sum of their parts? We’ve studied each factor alone. Now we need to know how they work together.
But here’s the bottom line: you don’t need to wait for the future. The tools you need are already here. Move more. Eat plants. Avoid tobacco and excess alcohol. Protect your skin. Lose a little weight if you need to. These aren’t suggestions. They’re proven shields.
Frequently Asked Questions
Can I prevent cancer just by eating healthy?
Eating healthy helps-but it’s not enough alone. Cancer prevention works best when you combine diet with physical activity, weight management, avoiding tobacco, limiting alcohol, and sun protection. Studies show that people who follow at least three of these habits reduce their cancer risk by 18-21%. No single change is a magic bullet, but together, they create powerful protection.
Is chemoprevention right for me?
Chemoprevention-like aspirin or tamoxifen-is only recommended for people at high risk, such as those with strong family histories or genetic mutations. For most people, lifestyle changes are safer, more effective, and have fewer side effects. Talk to your doctor if you have a personal or family history of cancer. They can use risk models to help decide if chemoprevention makes sense for you.
How much exercise do I really need to lower cancer risk?
You don’t need to train like an athlete. Aim for 150 minutes of moderate activity per week-that’s 30 minutes, five days a week. Brisk walking counts. Studies show this reduces colon cancer risk by 24% and breast cancer by 12-20%. Even 10-minute walks after meals help. The key is consistency, not intensity. Moving more than you do now is the first step.
Does alcohol really cause cancer even in small amounts?
Yes. There’s no safe level of alcohol when it comes to cancer risk. Each additional drink per day increases breast cancer risk by 7-12% and esophageal cancer by 20-30%. Even one drink a day raises your risk. The guidelines say men should have no more than two drinks a day and women no more than one-but cutting back to zero gives the most protection.
Can I reverse cancer risk if I’ve smoked for years?
Absolutely. Within 20 minutes of quitting, your heart rate drops. After five years, your risk of mouth, throat, and esophageal cancers is cut in half. After 10 years, your lung cancer risk is half that of a current smoker. Your body heals faster than most people think. Quitting at any age gives you benefits. The sooner, the better-but it’s never too late.
Why don’t doctors talk more about cancer prevention?
A 2023 study found only 38% of primary care doctors consistently discuss all seven cancer prevention guidelines during annual visits. Reasons include time limits, lack of training, and uncertainty about how to help patients make changes. But that’s changing. The American Medical Association’s STEADI toolkit and ASCO’s ‘Prevention First’ initiative are training doctors to have these conversations. If your doctor doesn’t bring it up, ask. You’re the most important person in your health.
Next Steps: What to Do Today
Don’t wait for tomorrow. Start with one thing.
- If you smoke: Set a quit date this week. Use free resources like smokefree.gov or call 1-800-QUIT-NOW.
- If you’re inactive: Walk for 10 minutes after dinner today. Add 5 more minutes each day.
- If you don’t eat enough veggies: Add one extra serving to lunch or dinner today. Try roasted broccoli, spinach in an omelet, or carrots with hummus.
- If you drink alcohol: Skip it one day this week. Notice how you feel.
- If you’re overweight: Aim to lose 5% of your body weight. That’s 5-10 pounds for most people. It’s easier than you think.
Small steps. Daily. That’s how prevention works. Not with grand gestures. With quiet, consistent choices. Your future self will thank you.

