Medication Switching Decision Calculator
How This Tool Works
This calculator helps you compare medications by showing how each option aligns with what matters most to you. Enter your personal priorities, and we'll show which medication best matches your values.
Your Priorities
Rate each factor on a scale of 1-10 (10 = most important)
Medication Comparison
Drug A (Metformin)
0-5% weight gain
Drug B (SGLT2 Inhibitor)
10-15% weight gain
2% risk
1% risk
5% risk
25% risk
Minimal protection
30% lower risk
Your Recommended Choice
Enter your priorities and click "Calculate My Best Match" to see your personalized recommendation
Why switching medications isn’t just a doctor’s call
Changing a medication isn’t like switching your phone plan. One wrong move can mean worse side effects, hospital visits, or even life-threatening reactions. And yet, nearly half of all patients stop their new meds within a year-not because they didn’t work, but because they didn’t understand the trade-offs. That’s where decision aids come in. These aren’t fancy apps or flashy brochures. They’re structured tools that help you and your doctor weigh what matters most to you when switching meds.
What exactly is a medication decision aid?
A decision aid is a tool built on real medical data. It shows you the facts: if you switch from Drug A to Drug B, what are the odds you’ll gain weight? How much does your risk of a stroke go down? What’s the chance you’ll get dizzy or have stomach pain? These aren’t guesses. They’re based on studies of thousands of people.
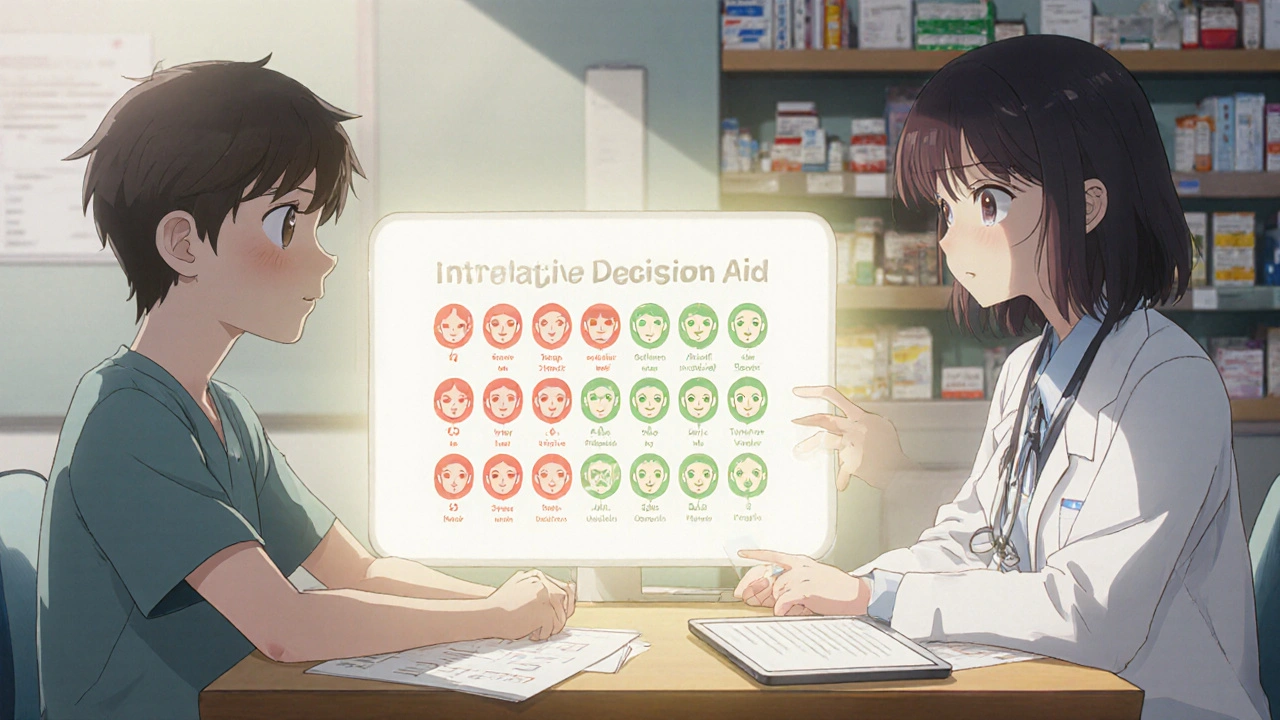
Good decision aids don’t just list side effects. They show them visually. Think of icon arrays-100 little faces, where 15 are colored red to show how many people on a certain drug had nausea. Or a simple table comparing two drugs side by side:
| Side Effect | Drug A (Metformin) | Drug B (SGLT2 Inhibitor) |
|---|---|---|
| Weight gain | 0-5% chance | 10-15% chance |
| Low blood sugar | 2% chance | 1% chance |
| Urinary tract infections | 5% chance | 25% chance |
| Heart protection | Minimal | 30% lower risk |
This kind of clarity turns vague fears into concrete numbers. You’re not just hearing ‘this drug might cause weight gain.’ You’re seeing that 1 in 7 people on Drug B gain weight, while only 1 in 20 on Drug A do.
How decision aids beat old-school advice
Traditionally, doctors hand you a pamphlet or say, ‘This one works better.’ But pamphlets don’t ask you what you care about. Maybe you hate taking pills multiple times a day. Maybe you’re terrified of kidney issues because a family member had one. Maybe cost is the biggest barrier.
Decision aids force you to pick what matters. They’ll ask: ‘On a scale of 1 to 10, how important is avoiding weight gain?’ Then they’ll show you how each option stacks up. One study found that when patients used these tools, they were 32% more likely to remember the key facts six months later. That’s not a small win. It’s the difference between sticking with a med or quitting because you forgot why you started.
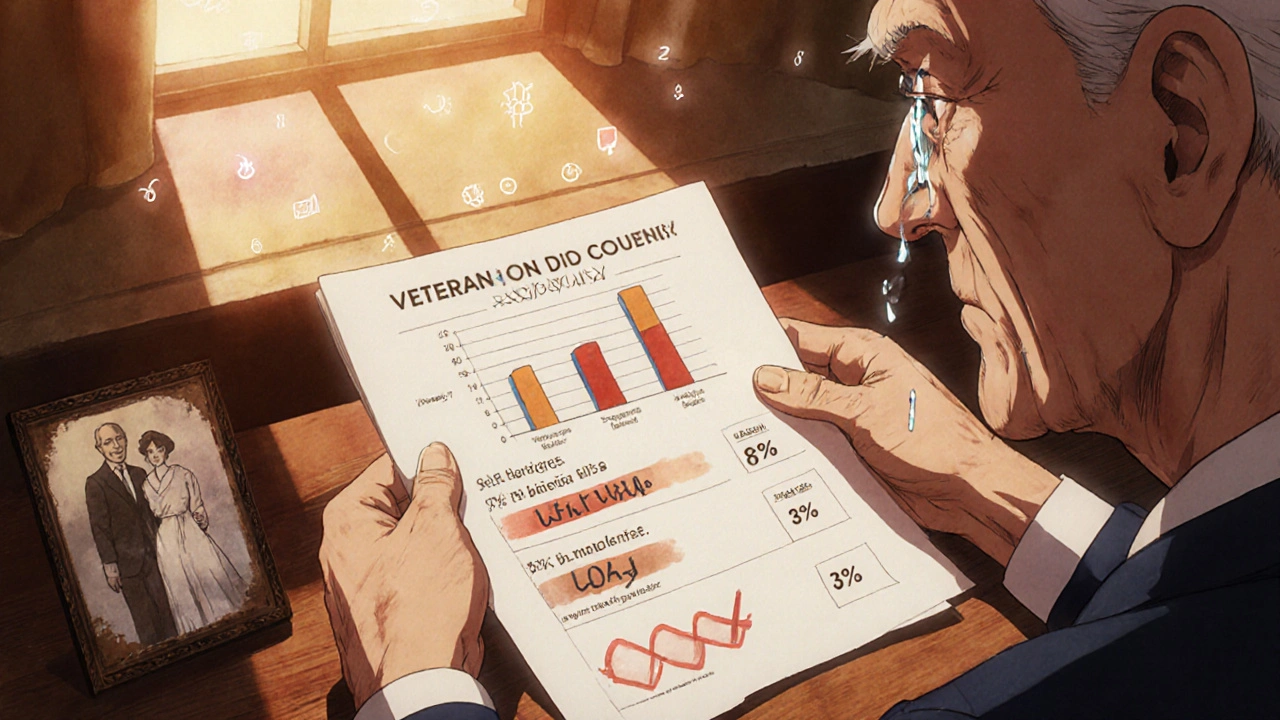
Real stories: When the numbers changed everything
One veteran in the VA system was on warfarin for blood clots. His doctor suggested switching to a newer drug. He didn’t know what the difference was-until he used the decision aid. It showed him: out of 100 people like him, 8 on warfarin had serious bleeding each year. On the new drug? Only 3. But the new drug cost $300 more per month. He had to decide: was avoiding 5 bleeding events worth the extra cost? He chose to stay on warfarin. He said, ‘I didn’t realize the risk was that low. I was scared for nothing.’
Another patient with depression was being pushed to switch antidepressants. Her old med made her sleepy. The new one was supposed to help energy. But the decision aid showed her that 1 in 3 people on the new drug had severe nausea. She had already struggled with eating after her cancer treatment. She said, ‘I can’t handle that. I’d rather be tired than sick to my stomach.’ She stayed on her old med-and felt better because she was in control.
When decision aids don’t work
These tools aren’t magic. They don’t help if you’re in an emergency. If your blood pressure spikes or you’re having a seizure, you need a doctor’s quick call-not a 10-minute interactive tool.
They also struggle when patients have memory problems or trouble understanding numbers. A study found that if someone scored below 24 on a basic mental test, the aid didn’t improve their decisions. That’s not a flaw in the tool-it’s a sign that some people need more support, not just more data.
And sometimes, the tool itself overwhelms. One patient told a Mayo Clinic researcher: ‘It had too many numbers. I felt like I was back in math class.’ That’s why the best aids let you skip ahead, focus on just one side effect, or hear the info spoken aloud.
What your doctor needs to know
Doctors aren’t trained to use these tools automatically. Many still rely on quick chats during 15-minute visits. But using a decision aid properly takes time. Studies show it adds 7 to 12 minutes to a visit. That’s why only 29% of primary care clinics use them regularly.
But when they do, results improve. Patients feel less stressed about decisions. They’re more likely to stick with their meds. And doctors report fewer follow-up calls asking, ‘Why did you give me this?’
The VA, Mayo Clinic, and Ottawa Hospital have all built free, public libraries of these tools. You don’t need a special login. Just ask your doctor: ‘Do you have a decision aid for switching my med?’ If they say no, ask if they can pull up one from the VA’s website. Many are available online for free.

How to use a decision aid before your appointment
Don’t wait until you’re in the exam room. Get the tool early. Most are web-based or app-based. Spend 10-15 minutes with it before your visit. Do this:
- Read the risk numbers. Don’t just skim. Look at the icon arrays.
- Answer the value questions honestly. What scares you? What’s non-negotiable?
- Write down one question you still have.
- Bring your answers to the appointment.
This turns your visit from a lecture into a conversation. You’re not just receiving advice-you’re co-making the decision.
What’s new in 2025
Now, some tools are getting smarter. In 2024, Intermountain Healthcare launched a version that adapts to how you learn. If you respond better to visuals, it shows more charts. If you prefer words, it gives you more explanations. It even remembers your past answers so it doesn’t repeat the same info.
The FDA is also stepping in. Starting in 2025, any decision aid used in Medicare plans must prove it actually helps patients understand their options. That means fewer misleading tools and more honest ones.
Bottom line: You have a right to understand
Switching meds is a big deal. It’s not just about what works in a study. It’s about what works for you-your body, your life, your fears. Decision aids don’t make the choice for you. They give you the facts, the context, and the space to decide without pressure.
If you’re being asked to switch meds, ask for a decision aid. If your doctor doesn’t have one, ask where to find it. You’re not being difficult. You’re being smart. And that’s exactly what these tools were made for.
Are medication decision aids only for serious conditions?
No. Decision aids work for any medication switch where there’s more than one valid option. That includes antidepressants, blood pressure pills, diabetes meds, cholesterol drugs, and even pain relievers. The key is whether the choice depends on your personal priorities-not just clinical guidelines. If your doctor says, ‘Either one is fine,’ that’s when you need the tool.
Can I use a decision aid without my doctor’s help?
Yes, you can explore them on your own. Many are free and public, like those from the Ottawa Hospital or VA. But they’re designed to be used with your doctor-not instead of them. The goal is to start a better conversation, not make a decision alone. Bring what you learn to your appointment and ask, ‘Does this match what you’d recommend?’
What if the decision aid says one drug is better, but my doctor recommends another?
That’s normal. Decision aids show evidence-based options, but your doctor knows your full history-your kidney function, allergies, other meds, even your work schedule. The tool helps you understand the trade-offs, but your doctor adds context. If there’s a mismatch, ask: ‘What am I missing? Why do you think this option is better for me specifically?’
Do decision aids cost money?
No. The most reliable ones are made by hospitals and government agencies and are free to use. Avoid commercial tools that ask for payment or try to sell you a product. Stick to sources like the Ottawa Hospital Research Institute, Mayo Clinic, or the U.S. Department of Veterans Affairs. These are updated regularly and reviewed by medical experts.
How do I know if a decision aid is trustworthy?
Check the source. Trusted ones are made by universities, hospitals, or government health agencies. Look for dates-ideally updated within the last two years. Avoid tools that only highlight benefits or hide side effects. Good ones show both sides clearly. If it says ‘90% effective’ without explaining what that means, walk away.
What if I still feel confused after using the aid?
That’s okay. Decision aids don’t have to make everything clear right away. If you’re still unsure, ask your doctor to explain one part again. Or ask for a follow-up appointment. You can also bring a friend or family member to help you process the info. It’s not a test-you’re not expected to understand everything immediately. The goal is to reduce anxiety and feel heard.