People assume generic drugs are just cheaper copies of brand-name pills. That’s mostly true - but not in the way most think. The active ingredient? Identical. The way it works in your body? The same. So why do some patients swear their generic blood pressure pill gives them headaches, or their generic thyroid medicine makes them feel off? The answer isn’t in the chemistry. It’s in the inactive ingredients.
Generics Aren’t the Problem - The Excipients Are
Generic drugs must contain the exact same active ingredient, dose, and route of delivery as the brand-name version. That’s not a suggestion. It’s a legal requirement enforced by the FDA. For most medications, this means the interaction profile is identical. If your brand-name simvastatin interacts with grapefruit juice, so does the generic version. If your brand-name warfarin reacts with vitamin K-rich foods, the generic does too. But here’s what most people don’t know: generics can use different fillers, dyes, binders, and preservatives. These are called excipients. They don’t treat your condition. They just hold the pill together, help it dissolve, or make it easier to swallow. But for some people, they cause problems. A 2021 case in the Journal of the American Pharmacists Association involved a patient who switched from a brand-name levothyroxine to a generic version and suddenly developed bloating and diarrhea. The brand version used no lactose. The generic did. The patient had a mild lactose intolerance - never noticed before because the brand pill didn’t contain it. Once switched, the reaction started. The drug worked fine. The problem was the filler. This isn’t rare. A 2022 study in the Journal of Clinical Pharmacy and Therapeutics tracked 127 cases where patients reported different side effects with generics. Only 17 - less than 14% - had any real pharmacological difference. The rest? Allergic reactions to dyes, stomach upset from new binders, or psychological reactions because they believed generics were inferior.Why the Confusion? Perception Over Science
There’s a powerful myth out there: generics are less effective. It’s not true. But it’s widespread. A 2022 Kaiser Family Foundation survey found nearly half of patients believed generics work differently than brand-name drugs. Over a quarter said they experienced more side effects with generics. But when researchers checked medical records, only 3.7% of those reports matched actual physiological changes. The rest? Nocebo effect. That’s when expecting a negative outcome makes you feel it. If you’re told your new generic pill is "cheap" or "not the same," your brain can start creating symptoms - even if the drug is identical. Pharmacists report this constantly. In one 2023 survey, 62% of patients said they believed generics interact differently. Only 18% of pharmacists had ever seen a real case. Most of the time, when someone says their generic blood thinner is "not working," it’s because they missed a dose, changed their diet, or switched between different generic brands without realizing it.When Generics Really Do Require Caution
There are exceptions. For drugs with a narrow therapeutic index - meaning the difference between a safe dose and a dangerous one is tiny - even small changes matter. These include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Digoxin (heart medication)
- Phenytoin (seizure control)
What You Can Do to Stay Safe
You don’t need to avoid generics. They’re safe, effective, and save billions every year. But you do need to be smart.- Stick with one generic brand. If you’re on a narrow therapeutic index drug, ask your pharmacist to fill your prescription with the same manufacturer each time. Don’t let them switch without telling you.
- Check the label. Generic labels list all inactive ingredients. If you’re allergic to lactose, gluten, or certain dyes, read them. If you’re unsure, call your pharmacist.
- Don’t assume new side effects mean the drug isn’t working. If you feel different after switching to a generic, write down what changed - when, how, and how bad. Bring it to your doctor. It might be the excipient, not the drug.
- Keep a medication log. Note every drug, dose, and when you switch brands. This helps your doctor spot patterns. Was your INR stable until you switched from Generic A to Generic B? That’s data.
- Ask about alternatives. If you’re having reactions, your pharmacist might know of another generic version with different fillers. Or your doctor might suggest a brand-name version if it’s medically necessary.
Why This Matters More Than You Think
Over 90% of prescriptions in the U.S. are filled with generics. That’s not just about cost - it’s about access. Without generics, millions couldn’t afford their meds. But misinformation is costing lives - not because generics are unsafe, but because people stop taking them. A 2023 Health Affairs analysis found that 1.2 million unnecessary brand-name prescriptions are filled each year because patients fear generics. That adds up to $8.7 billion in extra costs. And for what? A myth. The real issue isn’t the science. It’s the silence. Patients aren’t told about excipients. Pharmacists don’t always explain the switch. Doctors assume patients understand generics are identical. They’re not.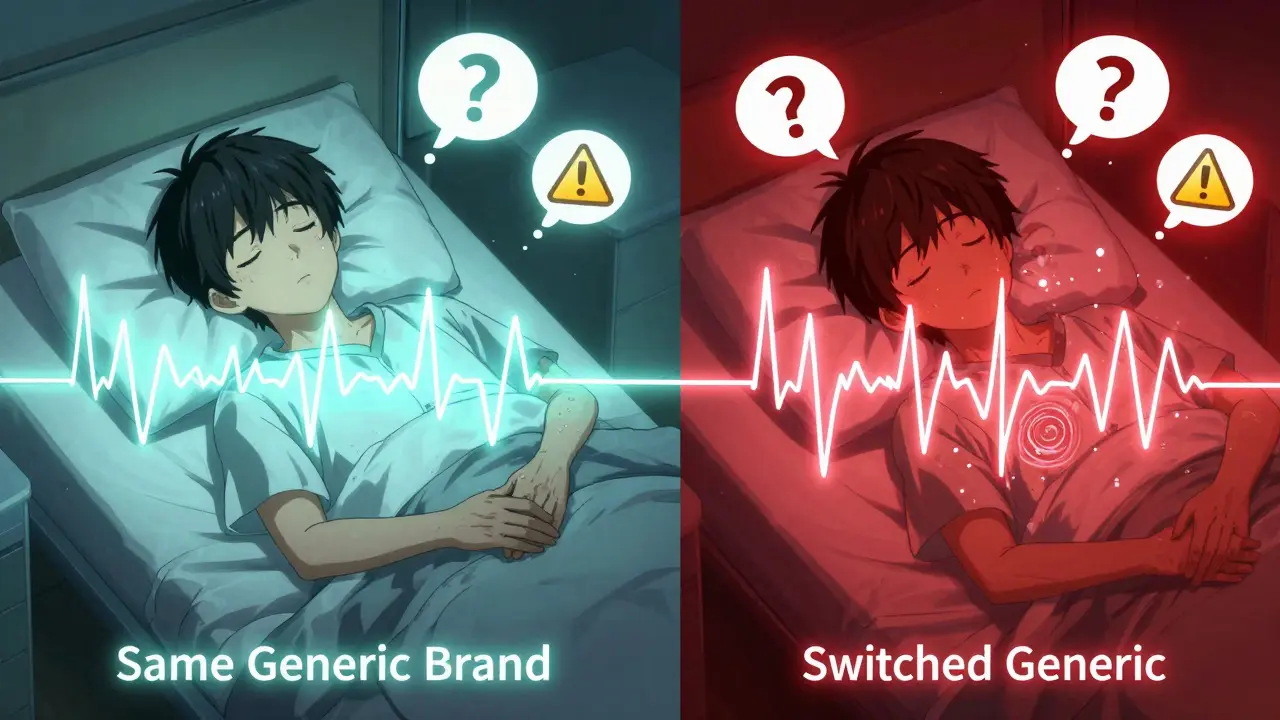
What’s Being Done
The FDA launched a $15 million public education campaign in January 2024 called "Generics Awareness." It’s targeting the biggest myths: that generics are weaker, less safe, or interact differently. The American Medical Association is updating its guidelines to require doctors to explain generics to patients during prescribing. Pharmacies are training staff to ask patients: "Have you switched generics recently?" before adjusting doses. In Australia, where I’m based, the Therapeutic Goods Administration has similar rules to the FDA. Generics must prove bioequivalence. Excipients are listed. And pharmacists are trained to flag switches for high-risk drugs.Bottom Line
Generic drugs don’t interact differently because they’re generic. They interact the same way because they contain the same active ingredient. The rare problems come from fillers, not the medicine. The bigger problem is the fear - fueled by confusion, not science. If you’re on a critical medication, stay consistent. Know your fillers. Ask questions. Don’t assume a new side effect means the drug is failing. And don’t let myths keep you from saving money - or worse, from taking your medicine at all.Do generic drugs have the same drug interactions as brand-name drugs?
Yes. The active ingredient in a generic drug is identical to the brand-name version, so drug interactions - whether with other medications, food, or medical conditions - are the same. The FDA requires generic manufacturers to include the same interaction warnings as the brand-name product. Any differences in reactions are almost always due to inactive ingredients or psychological factors, not the drug’s pharmacology.
Can inactive ingredients in generics cause side effects?
Yes, but rarely. Inactive ingredients like lactose, dyes, or preservatives can trigger allergic reactions or digestive upset in sensitive individuals. For example, a patient allergic to lactose might react to a generic levothyroxine that contains it, even if the brand version doesn’t. These are not drug interactions - they’re reactions to fillers. Always check the ingredient list on the label.
Why do some people feel different on a generic version?
Most often, it’s the nocebo effect - feeling worse because you expect to. Other times, it’s switching between different generic manufacturers, each using different fillers. Rarely, it’s a dosing error or an undiagnosed change in health. If you feel different after switching, track your symptoms and talk to your pharmacist or doctor. Don’t assume the drug isn’t working.
Should I avoid generics for blood thinners like warfarin?
No - but be consistent. Warfarin has a narrow therapeutic range, so even small changes in absorption can affect your INR. The FDA requires stricter bioequivalence standards for generics of these drugs. The key is to stick with the same generic manufacturer. Switching between brands can introduce variability in fillers, which may affect absorption in sensitive individuals. Always inform your doctor if you switch generics.
How can I find out what’s in my generic medication?
The package insert or pharmacy label lists all active and inactive ingredients. If it’s not clear, ask your pharmacist. They can tell you the manufacturer and provide a full ingredient list. Some pharmacies also offer online access to this info. Don’t rely on the brand-name label - generics have their own labeling, but the active ingredient is always the same.
Are there any generics that are not approved by the FDA?
All legally sold generics in the U.S. must be FDA-approved. However, some online pharmacies - especially those based overseas - sell unapproved or counterfeit versions. Always fill prescriptions through licensed pharmacies. If a generic looks different or costs too little, it might not be legitimate. Check the FDA’s website for approved generic drug lists if you’re unsure.

