Medication Safety Checker
Check if your symptoms could indicate a dangerous medication reaction. This tool identifies immediate actions based on the article's warning signs.
When you take a new medication, you expect it to help - not hurt. But sometimes, the very drug meant to fix one problem can trigger another, far more serious one. The truth is, dangerous medication side effects don’t always come with a warning label you can see coming. Many start quietly - a slight rash, a weird feeling in your chest, a sudden dizzy spell - and then escalate fast. Knowing what to look for could save your life.
What Makes a Side Effect Dangerous?
Not all side effects are created equal. A dry mouth, mild drowsiness, or an upset stomach? Those are common and usually harmless. But when a reaction involves your heart, lungs, liver, or immune system, it’s a different story. The FDA defines a serious side effect as one that leads to death, hospitalization, disability, or permanent damage. In 2022 alone, adverse drug reactions sent over 1.3 million people to the emergency room in the U.S. and caused nearly 128,000 deaths. The biggest danger isn’t always the drug itself - it’s how quickly the reaction spreads. A rash that shows up days later might be annoying. But if it’s paired with swelling in your throat or trouble breathing? That’s an emergency. Anaphylaxis, a severe allergic reaction, can kill within minutes. And it doesn’t always happen right after you take the pill. Sometimes, it sneaks up hours or even days later.Red Flags That Demand Immediate Action
There are five warning signs that should make you stop what you’re doing and call 911 right away:- Difficulty breathing or wheezing - Even if it feels like a cold, if it comes on suddenly after taking medicine, treat it like an emergency. This could mean your airways are closing.
- Swelling of the face, lips, tongue, or throat - This is a classic sign of anaphylaxis. Your skin might look normal, but inside, your body is going into shock.
- Chest pain or irregular heartbeat - Feeling like your heart is racing, fluttering, or skipping beats? Especially if it’s over 100 beats per minute or you feel faint, this could signal a dangerous heart rhythm. Some medications, including certain antibiotics and antidepressants, can trigger this.
- Unusual bleeding or bruising - If you’re bruising for no reason, or bleeding from your gums, nose, or stool, your blood may not be clotting properly. This can happen with blood thinners, NSAIDs, or even some antibiotics.
- Seizures or loss of consciousness - Any sudden change in mental state, confusion, or convulsions after taking medicine is a red flag. This often points to toxicity in the brain or nervous system.
Less Obvious, But Just as Dangerous
Some life-threatening reactions don’t scream for attention. They whisper. And by the time you notice, it’s too late.- Yellowing skin or eyes (jaundice) - This isn’t just a sign of being tired. It means your liver is struggling to process the drug. Medications like statins, acetaminophen, or semaglutide (Ozempic, Wegovy) can cause liver damage that builds up slowly. Left unchecked, it can lead to liver failure.
- Dark urine or no urine at all - Your kidneys are filtering your blood. If you stop making urine, or your pee turns tea-colored, you could be developing acute kidney injury. This is common with NSAIDs, certain antibiotics, and contrast dyes used in imaging tests.
- High fever with rash and swollen lymph nodes - This could be DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms). It’s rare, but deadly. It often starts with a rash, then fever, swelling, and organ inflammation. Most cases show up 2-6 weeks after starting the drug.
- Severe stomach pain with vomiting - If you’re on a weight-loss drug like tirzepatide (Mounjaro) or semaglutide, this could mean pancreatitis. The pain is sharp, constant, and often radiates to your back. Without treatment, mortality rates can hit 30%.
Why Timing Matters More Than You Think
The difference between a bad reaction and a fatal one is often how fast it progresses. Common side effects like nausea or dizziness usually appear within hours and stay stable. Dangerous ones? They spike. If you take a new medication and within 1-2 hours you feel your throat tightening, your skin breaking out in hives, or your heart pounding - don’t wait. Call 911. If symptoms show up after a day or two, but keep getting worse - don’t wait until tomorrow. Call your doctor today. A 2023 study in the Journal of the American Medical Association found that 6.7% of all hospital admissions were due to drug reactions - and most of those could have been prevented if the first signs had been caught early. The key isn’t just recognizing the symptom. It’s recognizing the pattern: new + worsening + unexpected.Who’s at Highest Risk?
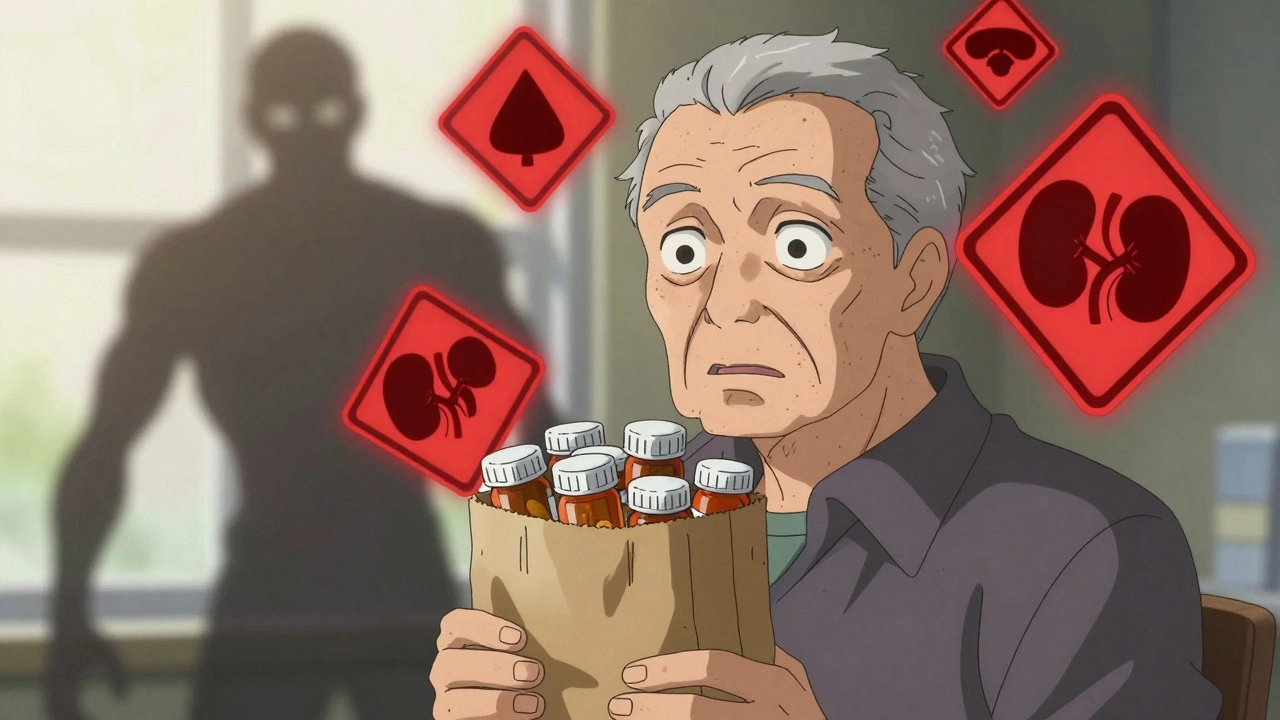
Some people are more vulnerable than others. If you fall into any of these groups, be extra careful:- Adults over 65 - Your body processes drugs slower. You’re 2.7 times more likely to have a dangerous reaction than someone younger.
- People taking five or more medications - This is called polypharmacy. The more drugs you take, the higher the chance they’ll clash. One study showed this increases dangerous side effect risk by 300%.
- Those with kidney or liver disease - These organs break down drugs. If they’re not working right, the medication builds up in your system and becomes toxic.
- People with a history of allergies - If you’ve had a reaction to one drug, you’re more likely to react to others, even if they’re in a different class.
What You Should Do - Step by Step
When you notice something off, don’t panic. Do this:- Stop taking the medication - But only if you’re sure it’s the cause. Never stop a prescription drug like blood pressure meds or antidepressants without talking to your doctor first. Abruptly stopping can cause seizures, heart attacks, or severe withdrawal.
- Call your doctor or pharmacist - Tell them exactly what you’re feeling, when it started, and what meds you’re on. Include supplements and over-the-counter drugs. Many reactions come from hidden interactions.
- Bring all your meds to your next appointment - The Brown Bag Method works. Put every pill, capsule, and bottle in a bag and take it with you. Your provider can spot duplicates, dangerous combos, or look-alike drugs like insulin and heparin - which are often confused and cause deadly errors.
- Use a symptom tracker - Write down when symptoms happen, how bad they are, and what you took before. Apps like Medisafe or even a simple notebook help your doctor connect the dots.

What You Should Never Do
- Never ignore a new symptom - Even if it seems small. A tiny rash could be the first sign of DRESS syndrome. A slight headache could be a sign of bleeding in the brain.
- Never assume it’s ‘just a side effect’ - Doctors say the same thing all the time: ‘That’s normal.’ But normal doesn’t mean safe. If it’s new, unusual, or getting worse, push back.
- Never wait to see if it gets better - Dangerous reactions don’t resolve on their own. They get worse. Fast.
How Technology Is Helping
There’s new hope on the horizon. Mayo Clinic’s AI-powered safety dashboard now analyzes your age, weight, kidney function, and current meds to predict your risk of side effects with 89% accuracy. The NIH’s Pharmacogenomics Research Network tests your genes before prescribing certain drugs - like carbamazepine - and has cut severe reactions by 47%. Apple and the American Heart Association are now testing smartwatches that detect irregular heart rhythms caused by medications. These tools aren’t perfect - but they’re changing the game. The goal? To stop reactions before they start.Final Thought: Trust Your Body
You know your body better than any algorithm. If something feels wrong after you take a new pill - even if your doctor says it’s ‘common’ - listen to that gut feeling. Medications are powerful. They can heal. But they can also harm. The best defense isn’t a long list of side effects on a label. It’s awareness, action, and speaking up.What are the most common dangerous side effects of medications?
The most common dangerous side effects include severe allergic reactions (anaphylaxis), irregular heartbeat, chest pain, unusual bleeding or bruising, seizures, jaundice (yellowing of skin or eyes), sudden loss of urine output, and severe abdominal pain. These can lead to organ failure, heart attack, or death if not treated quickly.
How soon after taking a medication can a dangerous side effect appear?
Dangerous reactions can happen within minutes - like anaphylaxis - or take days to weeks. Allergic reactions often show up within an hour. Skin rashes or liver damage may take days or even weeks. If a symptom is new, worsening, and appears after starting a new drug, treat it as potentially dangerous until proven otherwise.
Can over-the-counter drugs cause dangerous side effects?
Yes. Common OTC drugs like ibuprofen, naproxen, and acetaminophen can cause internal bleeding, liver failure, or kidney damage - especially when taken long-term or with other medications. Even allergy pills and sleep aids can interact dangerously with prescription drugs.
Should I stop taking my medication if I think I’m having a side effect?
Only if it’s a life-threatening reaction like trouble breathing, swelling, or chest pain - then call 911 immediately. For less urgent symptoms, don’t stop cold turkey. Abruptly quitting drugs like beta-blockers, antidepressants, or steroids can cause dangerous withdrawal. Call your doctor first.
Are older adults more at risk for dangerous medication side effects?
Yes. Adults over 65 are 2.7 times more likely to experience dangerous side effects due to slower metabolism, reduced kidney function, and often taking multiple medications. About 44% of older adults take five or more drugs daily, which triples their risk of harmful interactions.
What should I bring to my doctor if I suspect a medication reaction?
Bring all your medications - prescriptions, over-the-counter drugs, vitamins, and supplements - in a bag. Include the names, dosages, and how often you take them. Also note when symptoms started, what they feel like, and whether they got worse after taking a specific pill. This is called the Brown Bag Method and helps doctors spot dangerous interactions.
Knowing the signs isn’t just helpful - it’s essential. Medications are tools. But like any tool, they can hurt if used without care. Stay alert. Stay informed. And never ignore a warning your body is sending.

