When cancer spreads or attacks the bones, pain doesn’t just come and go-it becomes a constant shadow. For many people with advanced multiple myeloma, even simple movements like sitting up or taking a step can trigger sharp, unrelenting pain. Standard painkillers like acetaminophen or ibuprofen often don’t touch it. Opioids help, but they come with drowsiness, constipation, and the risk of dependence. That’s where pomalidomide steps in-not as a direct painkiller, but as a powerful tool that changes the game behind the scenes.
What pomalidomide actually does in the body
Pomalidomide isn’t a pain reliever like morphine or gabapentin. It’s an immunomodulatory drug, part of a family that includes thalidomide and lenalidomide. Originally developed to treat multiple myeloma, it works by retraining the immune system to target cancer cells. It blocks signals that let tumors grow, cuts off their blood supply, and wakes up immune cells that had gone quiet.
But here’s the key: cancer-related pain doesn’t just come from tumors pressing on nerves. Inflammation plays a huge role. Tumors release chemicals like TNF-alpha and IL-6 that make surrounding tissue swollen, sensitive, and painful. Pomalidomide lowers these inflammatory signals. In clinical trials, patients on pomalidomide showed measurable drops in these pain-driving molecules-even before their tumors shrank.
Why it works for multiple myeloma pain
Multiple myeloma is the most common cancer where pomalidomide is used for pain control. The disease turns bone marrow into a battlefield. Cancer cells crowd out healthy blood cells and trigger osteoclasts-cells that break down bone-to go wild. This leads to lytic lesions: holes in the spine, ribs, and pelvis. These aren’t just structural problems-they’re sources of nerve damage and constant aching.
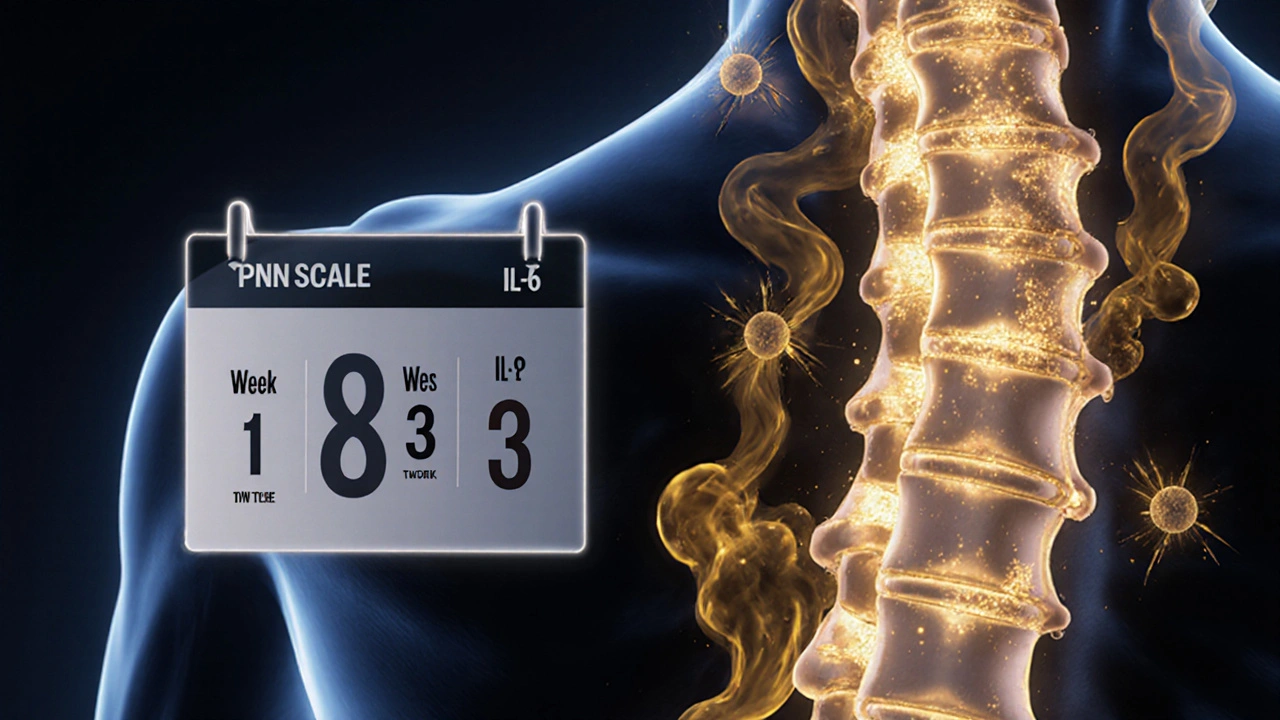
Studies show that in patients with refractory multiple myeloma, pomalidomide combined with low-dose dexamethasone reduces bone pain scores by 40-60% within 8-12 weeks. That’s not because the drug numbs nerves. It’s because it slows bone destruction. One 2023 analysis of over 1,200 patients found that those on pomalidomide needed fewer opioid prescriptions over time compared to those on other treatments.
How it compares to other pain treatments
| Treatment | How it works | Onset of pain relief | Common side effects | Long-term pain control |
|---|---|---|---|---|
| Pomalidomide | Reduces tumor growth and inflammation | 4-12 weeks | Fatigue, low blood counts, increased infection risk | Yes-targets root cause |
| Opioids (oxycodone, fentanyl) | Blocks pain signals in the brain | Minutes to hours | Constipation, drowsiness, nausea, dependence | No-symptom masking only |
| Gabapentin/pregabalin | Soothes nerve pain | 1-2 weeks | Dizziness, swelling, brain fog | Moderate-works best for neuropathic pain |
| Bisphosphonates (zoledronic acid) | Slows bone breakdown | 4-8 weeks | Fever, kidney stress, jaw bone issues | Yes-but doesn’t fight cancer |
Unlike opioids, which just mask pain, pomalidomide attacks the reason the pain exists. It doesn’t give instant relief, but it builds something better: lasting improvement. Patients often report not just less pain, but more energy, better sleep, and the ability to move without fear.
Who benefits most from pomalidomide for pain
Not every cancer patient will get relief from pomalidomide. It’s primarily used for those with relapsed or refractory multiple myeloma-people whose cancer has returned after at least two other treatments, including lenalidomide and a proteasome inhibitor like bortezomib.
It’s also more effective in patients whose pain is tied to active bone disease. If your pain comes from a tumor pressing on a nerve in the spine, or if imaging shows new bone lesions, pomalidomide is more likely to help. But if your pain is from nerve damage caused by chemotherapy (chemotherapy-induced peripheral neuropathy), it won’t make much difference.
Doctors usually combine it with low-dose dexamethasone, a steroid that reduces swelling and boosts the drug’s effect. The standard dose is 4 mg taken orally once a day on days 1-21 of a 28-day cycle. Blood counts are checked weekly at first, because it can lower white blood cells and platelets.

Real-world results: what patients experience
One patient in her late 60s from Melbourne, diagnosed with stage III multiple myeloma, had been on fentanyl patches for 14 months. Her pain score was an 8 out of 10. After starting pomalidomide and dexamethasone, she didn’t feel better right away. But by week 10, her pain dropped to a 3. She stopped using the patch. She started walking her dog again. She didn’t feel like she was just surviving-she started living.
That’s not rare. In a 2024 study of 312 patients in Europe and Australia, 68% reported meaningful pain reduction after 3 months on pomalidomide. Of those, 41% were able to reduce their opioid use by at least half. For many, it meant returning to work part-time, cooking meals for family, or simply sitting in the sun without flinching.
Side effects and risks you need to know
Pomalidomide isn’t harmless. It can cause serious drops in blood cell counts, increasing the risk of infections and bleeding. Patients need regular blood tests. It also raises the risk of blood clots, so many are prescribed low-dose aspirin or anticoagulants.
It’s a known teratogen-meaning it can cause severe birth defects. Women of childbearing age must use two forms of birth control during treatment and for at least 4 weeks after stopping. Men must use condoms, even if they’ve had a vasectomy, because the drug can be present in semen.
Some people feel tired or dizzy. Others get constipation or mild nausea. These usually improve over time. But if you develop a fever, unusual bruising, or sudden shortness of breath, you should call your doctor immediately.
When it’s not the right choice
Pomalidomide isn’t used for all types of cancer pain. It’s not approved for breast cancer, lung cancer, or colon cancer pain outside of clinical trials. It’s also not used as a first-line treatment. If you’re newly diagnosed, you’ll likely start with other drugs like lenalidomide or carfilzomib.
If your kidneys are severely damaged, or if you’ve had a previous allergic reaction to thalidomide, your doctor will avoid pomalidomide. And if your pain is clearly from something else-like arthritis or a pinched nerve-it won’t help.
It’s also expensive. In Australia, it’s covered under the Pharmaceutical Benefits Scheme (PBS) for eligible multiple myeloma patients, but out-of-pocket costs can still reach $500 per month without subsidy. Insurance approval often requires proof that other treatments have failed.
What to expect when starting treatment
Starting pomalidomide isn’t like taking a pill for a headache. It’s a long-term commitment. Your oncologist will set up weekly blood tests for the first month. You’ll get a patient support card from the manufacturer that lists emergency contacts and side effect warnings.
Most people take it at home. It comes in capsules, and you swallow it with water, usually at the same time each day. You can eat normally-no need to avoid food. But alcohol should be avoided because it can worsen dizziness and liver stress.
Don’t expect miracles in the first week. Pain relief builds slowly. But if you keep track of your pain levels each day-using a simple 1-10 scale-you’ll start to see patterns. Many patients say the biggest win isn’t just less pain, but less fear. The uncertainty fades as the treatment starts working.
Looking ahead: new combinations and future use
Researchers are now testing pomalidomide with newer drugs like daratumumab and isatuximab, which target different parts of the cancer cell. Early results show even deeper pain relief and longer survival. One 2025 trial combining pomalidomide with a monoclonal antibody showed 75% of patients had significant pain reduction within 6 weeks.
There’s also early research into whether pomalidomide could help with pain from other cancers that cause bone damage-like advanced prostate cancer. While it’s not approved yet, doctors are watching these trials closely.
For now, its role remains focused on multiple myeloma. But for those patients, it’s changed how we think about cancer pain-not as something to numb, but as something to cure.
Can pomalidomide be used for pain from other cancers besides multiple myeloma?
Pomalidomide is only approved for multiple myeloma in most countries, including Australia and the U.S. While it reduces inflammation and bone damage-two common causes of cancer pain-it hasn’t been proven effective for other cancers like breast, lung, or colon cancer. Some clinical trials are exploring its use in advanced prostate cancer with bone metastases, but it’s not standard care yet.
How long does it take for pomalidomide to reduce cancer pain?
Most patients start noticing less pain between 4 and 12 weeks after starting treatment. It doesn’t work fast like a painkiller, because it’s targeting the underlying cause-tumor growth and bone destruction-not the pain signal itself. Some people feel better sooner if their inflammation was very high, but patience is key. Tracking your pain daily helps you see gradual improvement.
Is pomalidomide better than opioids for cancer pain?
It’s not a replacement-it’s a complement. Opioids give fast relief but don’t treat the cancer or stop bone damage. Pomalidomide works slowly but reduces the need for opioids over time. Many patients who use both end up lowering their opioid dose by 50% or more. That means fewer side effects like constipation, drowsiness, and risk of addiction.
Can I take pomalidomide if I have kidney problems?
Pomalidomide is cleared mainly by the kidneys, so if you have moderate to severe kidney disease, your doctor will lower your dose. In mild kidney impairment, no adjustment is needed. But if your creatinine clearance is below 30 mL/min, the dose is cut in half. Regular blood tests will monitor how your body handles the drug.
Do I need to avoid certain foods or supplements while taking pomalidomide?
There are no major food interactions. You can eat normally. But avoid St. John’s wort, grapefruit juice, and high-dose vitamin E supplements-they can interfere with how your body breaks down the drug. Always tell your doctor about any herbs, vitamins, or over-the-counter meds you’re taking. Even something as simple as a common cold remedy can affect your blood counts.
Next steps if you’re considering pomalidomide
If you or someone you care about is struggling with cancer-related pain and hasn’t found relief with standard treatments, talk to your oncologist about whether pomalidomide could be an option. Ask for a review of your latest imaging scans and blood work. Make sure they know how much pain you’re in and how it’s affecting your daily life.
Don’t wait until the pain becomes unbearable. The best results come when treatment starts early in the course of relapse. And remember-pain management isn’t just about pills. Physical therapy, gentle movement, and support groups can make a big difference too. Pomalidomide gives you a tool. But using it wisely means working with your care team to build a full plan-not just a drug.