Every year, over 1.3 million people in the U.S. are hospitalized because of unexpected reactions to their medications. Many of these reactions don’t show up until it’s too late-dizziness after a new blood pressure pill, a sudden drop in heart rate from an antidepressant, or confusion from a painkiller. What if you could catch these signs before they become emergencies? That’s what remote monitoring for medication side effects is trying to do-using everyday devices and smart apps to watch for warning signs in real time.
How These Systems Actually Work
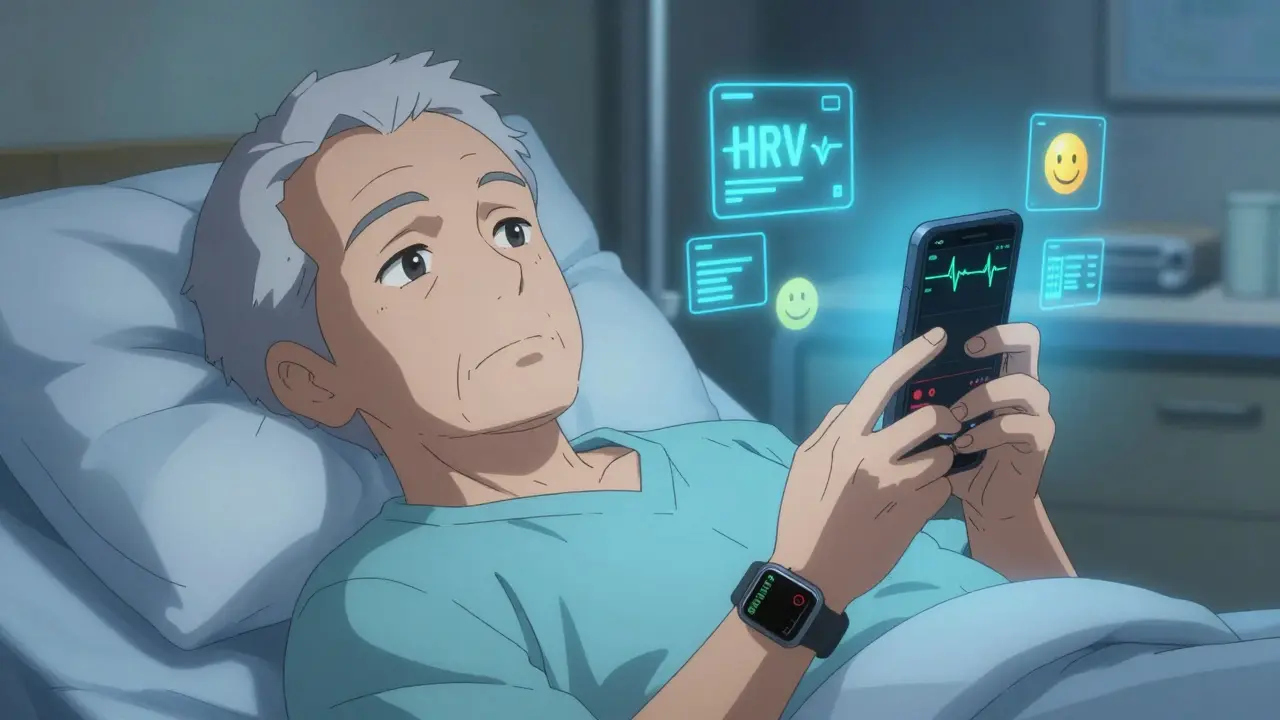
It’s not just about reminders to take your pills anymore. Modern platforms like Medisafe, AiCure, and Mango Health combine multiple data streams to spot problems early. They track when you take your medicine, then immediately start watching your body’s response. Your Apple Watch might detect a spike in heart rate. Your phone’s camera could notice you’re moving slower or blinking less-signs of drowsiness from a sedative. The app then cross-references those changes with what’s known about your specific drug. For example, if you start a new beta-blocker, the app knows that one common side effect is reduced heart rate variability (HRV). If your HRV drops more than 15% below your personal baseline for two full days, the system flags it. That’s not a guess-it’s based on clinical data from Massachusetts General Hospital. The same system might notice you’ve been reporting nausea in daily check-ins and combine that with a slight rise in your resting heart rate. Together, those signals point to a possible reaction, not just bad luck or a stomach bug.Top Platforms and What They Can Do
Not all apps are built the same. Here’s how the leading tools stack up:| Platform | Key Feature | Device Integration | Accuracy | Cost (Annual per Patient) |
|---|---|---|---|---|
| AiCure | AI facial analysis for ingestion and side effect detection | Smartphone camera only | 96.7% medication verification | $249 |
| Medisafe | HRV and heart rate monitoring with wearable sync | 78 devices (Apple Watch, Fitbit, etc.) | 88% sensitivity for cardiac side effects | $99 |
| Mango Health | NLP analysis of symptom reports against FDA database | Text input only | 89.3% accuracy in identifying drug-related symptoms | $79 |
| HealthArc | Adaptive Side Effect Detection Engine (ASDE) | 42 medical-grade devices | 91% correlation with clinical events | $199 (min. 50 patients) |
| Pill Identifier & Med Scanner | Pill recognition + symptom correlation | Smartphone camera | 94.6% pill ID accuracy | Free (in-app purchase for side effect alerts) |
AiCure is the most advanced at confirming you actually took your pill-using AI to watch your face as you swallow. But it’s expensive and designed mostly for clinical trials. Medisafe is the most balanced: affordable, widely compatible with consumer wearables, and trusted by hospitals. Mango Health is great if you’re good at tracking symptoms yourself, but it doesn’t monitor your body directly. HealthArc is powerful for clinics managing complex cases, but it’s overkill for individual use. And the Pill Scanner? It’s useful if you’re worried about grabbing the wrong pill, but it can’t tell if your body is reacting to it.
What They’re Missing-and Why It Matters
These tools are smart, but they’re not perfect. One big problem? False alarms. About 1 in 5 alerts are wrong. You might feel tired because you didn’t sleep well, not because your medication is causing drowsiness. But the app doesn’t know that. It just sees a change and flags it. That’s why so many doctors turn off alerts. In a 2025 AMA survey, 68% of providers admitted they’ve silenced side effect notifications because they were too noisy. There’s also a hidden bias. Early data from CMS shows these systems are less likely to flag side effects in older African American patients. Why? Because the algorithms were trained mostly on data from younger, white populations. The FDA now requires new apps to prove they work equally well across all age, race, and gender groups-but not all companies have caught up yet. And then there’s the data. Your heart rate, sleep patterns, and symptom logs are deeply personal. If that data leaks, it could be used against you-by insurers, employers, or even lenders. Right now, HIPAA doesn’t fully cover these apps unless they’re part of a hospital system. Many are just consumer apps with weak privacy policies. A 2025 KLAS survey found 72% of patients are worried their side effect history could be used to deny coverage.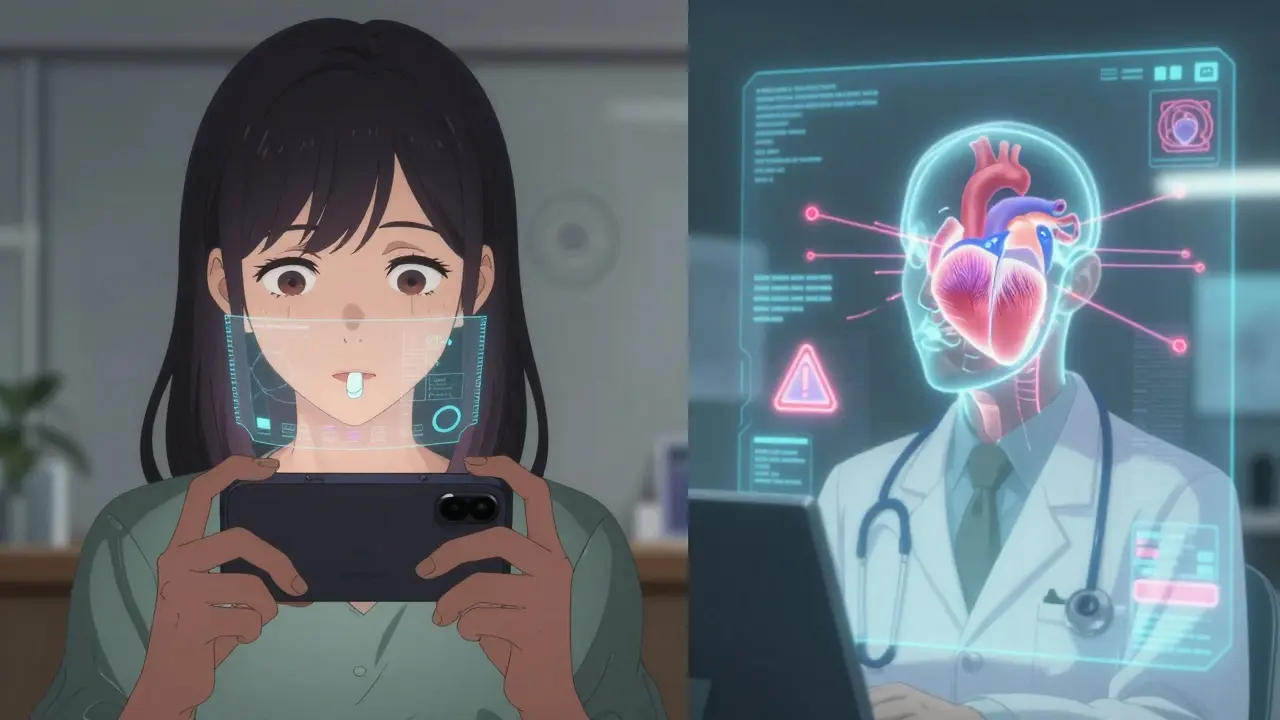
Who Benefits the Most?
This isn’t for everyone. But for certain groups, it’s life-changing.- People on multiple medications-especially seniors taking 5+ pills a day. One wrong interaction can send them to the ER.
- Patients on high-risk drugs: blood thinners, psychiatric meds, diabetes treatments, or heart medications.
- Those with chronic conditions like heart failure or kidney disease, where small changes in electrolytes or fluid balance can be dangerous.
- Caregivers managing medications for aging parents. Platforms like mySeniorCareHub now include drug interaction checkers that warn before a new pill is given.
At Geisinger Health, they assigned “digital health navigators” to help patients set up these tools. Their engagement rate jumped to 89%-nearly double the average. That’s the key: it’s not enough to give someone an app. Someone needs to walk them through it, answer questions, and make sure they’re not overwhelmed.
What’s Coming Next?
The next wave is even smarter. AiCure is testing “Digital Twin” technology-building a virtual model of how your body reacts to drugs based on your genetics, habits, and past responses. Early trials show it can predict your personal risk for side effects 43% better than standard models. The Mayo Clinic’s RIGHT Study is combining remote monitoring with genetic testing. They found that by identifying patients with certain gene variants, they could prevent 67% of adverse reactions before they even started. Imagine knowing your body can’t process a common painkiller before you’re prescribed it-that’s the future. The FDA is tightening rules for AI-based medical devices, which will likely cut false positives by 30-40% in the next two years. But that also means fewer apps will make it to market. The ones that do will be more reliable-but also more expensive and regulated.
How to Get Started
If you or a loved one is on high-risk meds and wants to try remote monitoring:- Ask your doctor if they use a monitoring platform. Many hospitals now offer Medisafe or similar tools as part of care.
- If not, check if your pharmacy or insurer partners with any. Some Medicare Advantage plans now cover RTM (Remote Therapeutic Monitoring) codes, which include side effect tracking.
- Start with a free app like Pill Identifier & Med Scanner to verify your pills, then upgrade to Medisafe if you have a compatible smartwatch.
- Don’t ignore alerts-but don’t panic either. Record what you were doing when the alert came up: Did you sleep poorly? Eat something new? Stressful day? Share that with your provider.
- Ask about data privacy. Find out who owns your data, how long it’s kept, and if it’s shared with third parties.
Remember: these tools don’t replace your doctor. They give your doctor better information. The goal isn’t to make you a data scientist-it’s to help you stay out of the hospital.
Frequently Asked Questions
Can these apps really prevent hospitalizations?
Yes-when used correctly. Studies show AI-powered monitoring can reduce severe adverse drug events by up to 37% in high-risk groups like heart failure patients. By catching early signs like abnormal heart rhythms or electrolyte shifts, doctors can adjust doses before things turn critical. The FDA and Deloitte estimate these systems could prevent over 1 million hospitalizations annually by 2027.
Are these apps covered by insurance?
Some are. Starting in 2025, Medicare and many private insurers began reimbursing for Remote Therapeutic Monitoring (RTM) codes that include medication side effect tracking. Patients can get $52-$67 per month billed to insurance if their provider uses an approved platform. Most consumer apps like Medisafe aren’t covered directly, but if your doctor prescribes it as part of your care plan, the cost may be absorbed.
Do I need a smartwatch to use these apps?
No, but you’ll get far more value with one. Apps like Mango Health only need your phone and your symptom entries. But to track heart rate, sleep, or activity changes that signal side effects, you need a wearable. Apple Watch Series 8 or newer, Fitbit Charge 6, and Garmin Venu 3 are the most compatible. If you don’t have one, your doctor might loan you a device through a hospital program.
What if the app gives me too many alerts?
Alert fatigue is real. Talk to your provider about adjusting thresholds. For example, if you’re on a blood pressure med and the app flags every minor HRV dip, ask them to raise the alert trigger from 15% to 20% deviation. Some platforms let you mute non-critical alerts. Never ignore all alerts-but don’t feel pressured to respond to every ping.
Is my data safe?
It depends. Apps connected to your hospital’s EHR (like Epic or Cerner) follow HIPAA rules. Standalone apps may not. Always check the privacy policy. Look for phrases like “encrypted end-to-end,” “no third-party sharing,” and “data ownership remains with you.” Avoid apps that sell your data or use it for ads. If you’re unsure, ask your doctor to recommend a trusted platform.