When you pick up a prescription, do you ever wonder if the generic version you're given is truly the same as the brand-name drug? It's a common question, especially when you notice a change in how you feel after switching. Some people swear they feel worse on generics. Others don't notice a thing. So, are adverse reactions more likely with generic medications? The answer isn't simple - but the data tells a clearer story than most people realize.
What Does "Bioequivalent" Really Mean?
The FDA requires generic drugs to be bioequivalent to their brand-name counterparts. That means the active ingredient must enter your bloodstream at the same rate and in the same amount - within 80% to 125% of the brand-name drug. On paper, that sounds strict. In practice, it leaves room for variation. For most drugs, that 20% wiggle room doesn't matter. But for medications with a narrow therapeutic index - like warfarin, levothyroxine, or phenytoin - even small changes in absorption can affect how well they work or how many side effects you get.Think of it like driving a car. If you're cruising on the highway, a slight change in fuel flow won't make a difference. But if you're navigating a tight turn at high speed, even a tiny shift in engine timing can throw you off. That's why doctors sometimes recommend sticking with one manufacturer for drugs like levothyroxine. It's not because generics are unsafe - it's because consistency matters more when the margin for error is razor-thin.
Do Generics Cause More Side Effects? The Data Says No - Mostly
A major 2018 study in PLOS Medicine looked at over 38 clinical trials involving more than 1 million patients. It compared outcomes for generic and brand-name versions of drugs used for heart disease, depression, osteoporosis, and diabetes. The results? No meaningful difference in effectiveness or safety. Patients on generics had the same rates of hospitalization, heart attacks, strokes, and death as those on brand-name drugs.Another study analyzed over 27,000 adverse event reports from the FDA's database. It found that while generics made up the majority of reports simply because they're used far more often, the rate of serious side effects per prescription was actually lower for generics than for brand-name drugs in several cases. For example, patients taking generic simvastatin were less likely to stop their medication due to side effects than those on the brand version - suggesting they tolerated it better.
One of the most surprising findings? For some drugs, the brand-name version caused more problems. A 2020 study in Nature Scientific Reports found that patients on branded bisoprolol had more major cardiac events than those on the generic. For simvastatin, 43% of brand-name users stopped taking it due to side effects - compared to just 28% of generic users.
The Real Culprit: Inactive Ingredients and the Nocebo Effect
If the active ingredient is the same, why do some people feel different? The answer often lies in the fillers - the inactive ingredients that give the pill its shape, color, or how fast it dissolves. A generic made in India might use a different starch or dye than the one made in the U.S. For most people, this doesn't matter. But for those with allergies, sensitivities, or digestive issues, even a tiny change can trigger symptoms.Then there's the nocebo effect - the flip side of the placebo effect. If you believe a generic drug is "inferior," your brain can start to interpret normal sensations as side effects. One study gave identical placebo pills to two groups. One group was told they were taking a brand-name drug. The other was told it was generic. The "generic" group reported significantly more side effects - even though both pills were sugar.
Another study showed that 54% of patients stopped taking a placebo pill labeled as "generic," compared to 33% who thought it was brand-name. That’s not pharmacology. That’s psychology.
Manufacturing Location Matters - But Not How You Think
You’ve probably heard that generics made in India or China are riskier. A 2022 study from Ohio State University claimed that Indian-made generics were linked to 54% more severe adverse events - including hospitalizations and deaths. But here’s the catch: the study looked at mature generics - drugs that have been on the market for years. These aren’t new products. They’re old, cheap, and often produced by companies with minimal oversight.The FDA inspects over 1,700 manufacturing facilities worldwide. More than 60% are outside the U.S. - 32% in India, 18% in China. That doesn’t mean they’re unsafe. It means they’re under pressure to produce cheap drugs at scale. The FDA’s own data shows that 12% of foreign facilities received "Official Action Indicated" ratings - meaning they had serious compliance issues. But that’s also why the FDA has ramped up inspections from 42 in 2010 to 317 in 2022.
The real issue isn’t country of origin. It’s quality control. A well-made generic from India is just as safe as one from the U.S. A poorly made one from anywhere is a risk.
Why Some Patients Report Real Problems
Patients with thyroid conditions, epilepsy, or depression often report drastic changes after switching to generics. Levothyroxine is the classic example. Many say they feel sluggish, anxious, or gain weight after switching. But here’s the twist: when researchers controlled for everything - diet, stress, other meds - the difference vanished. The problem? Switching between different generic manufacturers. One batch might use a slightly different binder. Another might dissolve a little slower. For someone with a sensitive metabolism, that’s enough to throw off hormone levels.The same goes for warfarin. Patients frequently report unstable INR levels after switching generics. But studies show it’s not the drug itself - it’s the change. Sticking with the same manufacturer reduces risk. That’s why some doctors write "Dispense as Written" on prescriptions for these drugs. It’s not because generics are dangerous. It’s because consistency prevents problems.
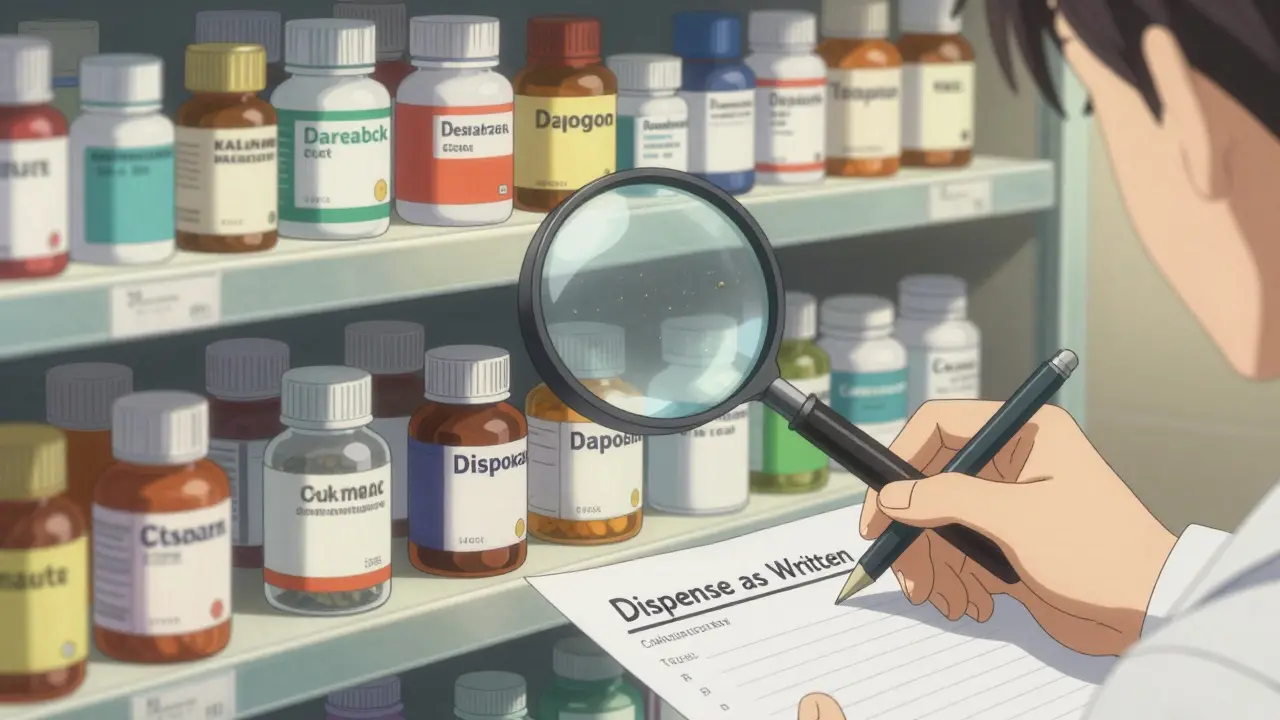
What Should You Do?
If you’re taking a generic and feel fine - don’t switch. If you’re switching and feel worse - talk to your pharmacist or doctor. Ask if you can go back to the previous version. Sometimes, it’s just a matter of sticking with one manufacturer.For drugs with a narrow therapeutic index, ask your provider to specify the manufacturer on your prescription. You don’t need to pay more. Many pharmacies can source the same generic from the same supplier.
And if you’re worried about side effects, educate yourself. A 2020 study found that patients who got a clear explanation about bioequivalence were 37% less likely to report side effects after switching. Knowledge reduces fear.