Sleep Aid Cognitive Impact Calculator
How Sleep Aids Affect Your Brain
This tool helps you understand the potential cognitive impact of your sleep medication based on the type of drug, duration of use, and your age.
More than 1 in 10 adults in the U.S. take sleep aids every night. But while these pills help you fall asleep faster, they might also be quietly dulling your thinking, memory, and focus-especially if you’re over 65. The problem isn’t just that they work too well. It’s that some of them interfere with the very brain functions you rely on to remember names, make decisions, or even walk safely across the street.
What’s Really in Your Sleep Pill?
Not all sleep aids are the same. The most common ones fall into four groups, and each has a different effect on your brain.- Benzodiazepines (like diazepam) and non-benzodiazepine hypnotics (like zolpidem/Ambien) work by boosting GABA, a calming brain chemical. But they don’t just calm you-they slow down your entire nervous system, including memory centers.
- Anticholinergics (found in some older antidepressants like trazodone, and even in over-the-counter sleep aids) block acetylcholine, a key neurotransmitter for learning and recall. These are the drugs most strongly linked to memory problems.
- Melatonin agonists (like ramelteon) mimic your body’s natural sleep hormone. They’re gentler, but their long-term cognitive impact isn’t well studied.
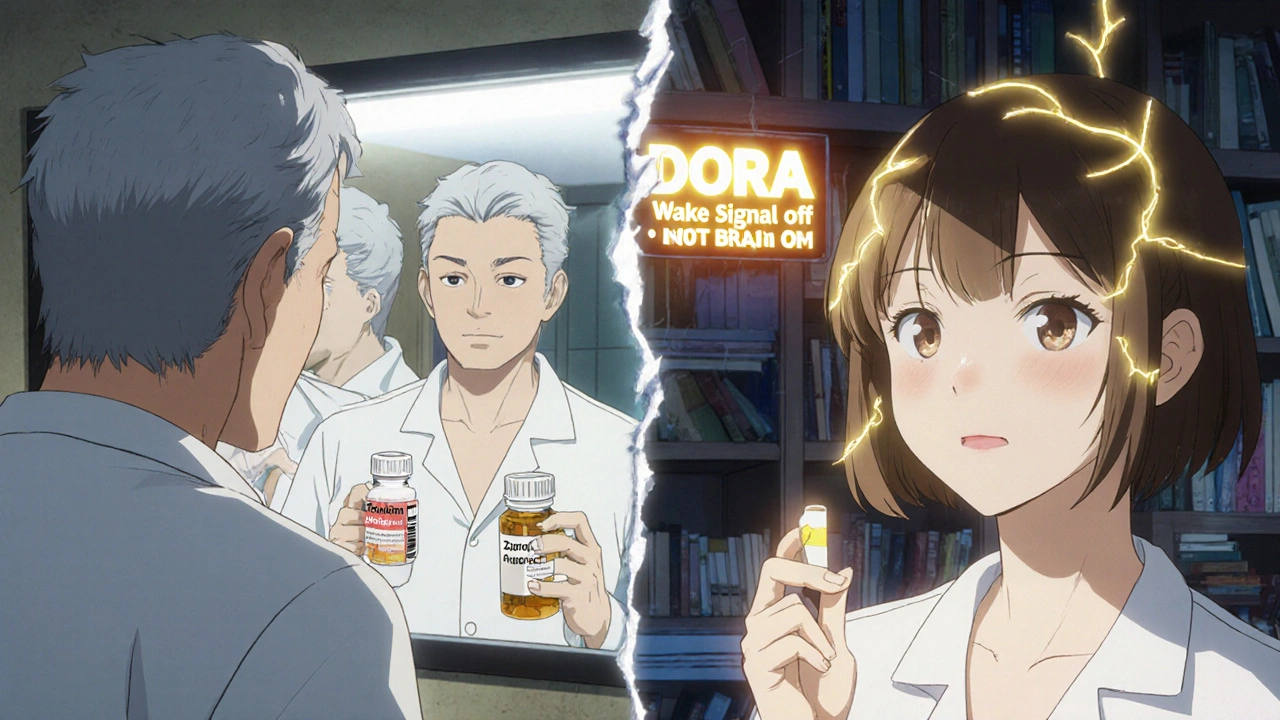
- Dual orexin receptor antagonists (DORAs) (like suvorexant/Belsomra and daridorexant/Quviviq) are newer. Instead of sedating your brain, they quiet the part that keeps you awake. Early research suggests they may not hurt thinking-and might even help protect it.
Here’s the catch: many doctors still prescribe benzodiazepines and trazodone as first-line treatments, even though the American Geriatrics Society’s 2023 Beers Criteria says they should be avoided in older adults. Why? Because they’re cheap, familiar, and patients feel better the next morning-until they don’t.
The Cognitive Cost: What the Science Shows
Studies tracking thousands of people over years reveal a clear pattern: not all sleep meds are created equal when it comes to your brain.A 2021 study of over 3,000 older adults found that white participants who took sleeping pills regularly had a 79% higher chance of developing dementia than those who rarely used them. But Black participants showed no increased risk-suggesting genetics, metabolism, or even how these drugs are prescribed may play a role.
Meanwhile, a 2023 study from Washington University found that suvorexant, a DORA, actually lowered levels of two proteins linked to Alzheimer’s disease-beta-amyloid and tau-in just two nights. That doesn’t mean it prevents dementia. But it’s the first time a sleep drug has shown a potential protective effect.
On the flip side, GABA-targeting drugs like zolpidem have been shown in controlled studies to reduce memory accuracy by 20% and slow reaction times by 15-20%. In monkeys, those effects were dose-dependent: higher doses = worse performance on cognitive tests. In humans, users report next-day brain fog, trouble concentrating, and even memory lapses during the night-like waking up having no recollection of getting up to use the bathroom.
And here’s the thing: the risk isn’t just for the elderly. A 2022 survey of 1,200 sleep aid users found that 58% quit their medication within six months-not because it didn’t work, but because of cognitive side effects. The top reasons? “Brain fog” (73%) and “trouble focusing” (68%).
Who’s Most at Risk?
Age is the biggest factor. As you get older, your liver and kidneys slow down. That means drugs stay in your system longer. A dose that’s fine for a 40-year-old can be dangerous for a 70-year-old.People with existing memory issues are also more vulnerable. If you’ve noticed yourself forgetting appointments, misplacing keys, or struggling to find the right word, adding a sleep aid could make it worse. And if you’re taking multiple medications-like blood pressure pills, antidepressants, or pain relievers-the risk of harmful interactions goes up.
One of the most dangerous combinations? Sleep aids with alcohol. Even one drink can double the sedative effect, increasing the chance of falls, confusion, and memory blackouts. Many users don’t realize this risk because doctors rarely mention it.
Women are also more likely to be prescribed these drugs, and they metabolize them slower than men. That means higher exposure over time-and potentially more cognitive impact.
What About the Newer Drugs?
DORAs like suvorexant and daridorexant are changing the game. Instead of shutting down your brain like a GABA drug does, they gently turn off the “wake signal” your brain sends at night. Think of it like dimming the lights instead of turning off the power.Users report fewer morning hangovers. On Drugs.com, 62% of suvorexant reviewers gave it 4 or 5 stars, often comparing it favorably to zolpidem. Only 38% of zolpidem users rated it 2 stars or lower-and the main complaints were memory lapses and grogginess.
Even more promising: DORA-22, still in preclinical trials, showed no cognitive impairment in animal studies while improving sleep. That’s huge. If it works in humans, it could be the first sleep aid that doesn’t just help you sleep-it lets you wake up thinking clearly.
What Should You Do If You’re Already Taking Sleep Aids?
If you’ve been on a sleep medication for months or years, don’t stop cold turkey. Withdrawal can cause rebound insomnia, anxiety, and even seizures in extreme cases.Instead, talk to your doctor about tapering. A slow reduction over 4 to 8 weeks is safest. Keep a sleep journal during this time-note how long it takes to fall asleep, how many times you wake up, and how you feel in the morning. That data helps your doctor adjust your plan.
And while you’re tapering, start cognitive behavioral therapy for insomnia (CBT-I). It’s not a quick fix-it takes 6 to 8 weekly sessions-but it’s the most effective long-term solution. Studies show it works better than pills, and the benefits last for years.
And you don’t need to see a therapist in person. Digital CBT-I programs like Sleepio have been proven just as effective, cost $300-$500, and are available 24/7. The American Academy of Sleep Medicine lists over 1,200 certified CBT-I providers nationwide.

The Bigger Picture: Sleep and Your Brain
Sleep isn’t just rest. It’s when your brain cleans out toxins, including the proteins that build up in Alzheimer’s disease. Chronic poor sleep isn’t just a symptom of dementia-it’s a risk factor. The Alzheimer’s Association estimates that fixing sleep problems could prevent 8% of dementia cases.That’s why experts are shifting away from pills and toward sleep hygiene. Avoid screens before bed. Keep your room cool and dark. Get sunlight in the morning. Move your body during the day. These aren’t just “tips.” They’re biological necessities.
And if you need something stronger? The future of sleep medicine isn’t in sedatives. It’s in drugs that respect your brain’s natural rhythms-not override them.
Final Thoughts: Is a Sleep Aid Worth It?
If you’ve tried everything else and still can’t sleep, a short-term sleep aid might help you reset your rhythm. But if you’re using it nightly for months, you’re trading better sleep for worse thinking.Ask yourself: Are you taking this pill because you can’t sleep-or because you’re afraid you won’t sleep without it? If it’s the latter, you’re not alone. But you’re not stuck. Better options exist.
Start by talking to your doctor. Bring this article. Ask: “Is this the safest option for my brain?” And if they push back, ask for a referral to a sleep specialist or CBT-I provider. Your memory-and your future self-will thank you.
Can sleep aids cause dementia?
Some sleep aids, especially benzodiazepines, anticholinergics, and long-term use of GABA-targeting drugs like zolpidem, are linked to a higher risk of dementia in older adults. However, newer drugs like suvorexant (a DORA) show no such risk-and early research suggests they might even reduce Alzheimer’s-related brain proteins. The risk depends heavily on the type of drug, how long you take it, and your age.
Do sleep aids make you forget things?
Yes, especially older drugs like zolpidem and benzodiazepines. These can cause temporary amnesia, where you don’t remember events from the night-like getting up to go to the bathroom or even driving. This is called “complex sleep-related behavior.” It’s rare but dangerous. Memory lapses are also common the next day as brain fog. DORAs are less likely to cause this.
Are over-the-counter sleep aids safer?
Not necessarily. Many OTC sleep aids contain anticholinergics like diphenhydramine (Benadryl) or doxylamine. These are linked to memory problems and increased dementia risk, especially in people over 65. Just because they’re sold without a prescription doesn’t mean they’re safe for long-term use. Melatonin supplements are generally safer but less effective for chronic insomnia.
What’s the best alternative to sleep medication?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s proven to work better than pills over the long term and has zero cognitive side effects. Digital programs like Sleepio offer the same results at a fraction of the cost. Other helpful habits include keeping a consistent sleep schedule, avoiding caffeine after noon, and getting morning sunlight to reset your body clock.
Can I stop taking my sleep aid cold turkey?
No. Stopping benzodiazepines or zolpidem suddenly can cause rebound insomnia, anxiety, tremors, or even seizures. Always work with your doctor to taper off slowly-usually over 4 to 8 weeks. During this time, start CBT-I to build sustainable sleep habits so you don’t fall back into the pill cycle.
Do sleep aids interact with other medications?
Yes, and it’s dangerous. Combining sleep aids with alcohol, opioids, antidepressants, or even some antibiotics can intensify sedation, slow breathing, and increase fall risk. Always give your doctor or pharmacist a full list of everything you take-including supplements and OTC meds. Anticholinergics in sleep aids can also interfere with medications for Parkinson’s, bladder control, or heart conditions.
Are newer sleep drugs like suvorexant really better?
Yes, for most people. Suvorexant and daridorexant don’t affect GABA or acetylcholine, so they’re less likely to cause brain fog, memory loss, or next-day impairment. User reviews show fewer complaints about grogginess. Early research also suggests they might lower Alzheimer’s-related brain proteins. They’re more expensive and require a prescription, but if you need a pill, they’re currently the safest option.

