Steroid eye drops are powerful tools for calming down serious eye inflammation-but they’re not harmless. Used the right way, they can save your vision. Used too long or without checkups, they can quietly damage it. If you’ve been prescribed these drops for uveitis, severe allergies, or post-surgery swelling, you need to know what’s really happening inside your eye-not just what your doctor tells you.
How Steroid Eye Drops Work
Steroid eye drops, like prednisolone acetate (Pred Forte), dexamethasone, and loteprednol, are synthetic versions of cortisol, the body’s natural anti-inflammatory hormone. When you put them in your eye, they block the chemical signals that cause redness, swelling, and pain. They’re not antibiotics-they don’t kill germs. They silence your immune system’s overreaction.
This makes them ideal for conditions like non-infectious conjunctivitis, uveitis (inflammation inside the eye), or corneal damage from burns or chemicals. In acute cases, they work fast. Many patients feel relief within 24 to 48 hours. For someone with painful, light-sensitive uveitis, these drops can mean the difference between seeing clearly and losing vision permanently.
The Hidden Dangers: Glaucoma and Cataracts
The biggest risk isn’t something you feel right away. It’s silent. And it’s common.
About 30 to 40% of people using steroid eye drops for more than two weeks will see their eye pressure rise. For 4 to 6%-called “steroid responders”-that pressure spikes dangerously high. Without treatment, this leads to steroid-induced glaucoma. The optic nerve gets crushed over time. Vision loss starts in the periphery. You won’t notice it until it’s too late.
And then there’s cataracts. Prolonged use-especially beyond 10 days-increases the risk of posterior subcapsular cataracts. These aren’t the foggy, age-related kind. They form right in the center of the lens, directly in your line of sight. You’ll notice blurry vision, glare at night, or colors looking faded. Unlike regular cataracts, these can develop in just a few months of steroid use.
One study showed that people on long-term steroid drops developed cataracts up to 10 years earlier than they otherwise would. For someone in their 40s or 50s, that means surgery they never expected so soon.
Who’s at Highest Risk?
Not everyone reacts the same way. Your risk depends on your history:
- You have a family history of glaucoma
- You already have high eye pressure or glaucoma
- You have diabetes
- You’ve used steroid drops before and had side effects
- You’re using high-potency drops like Pred Forte (not mild ones like Pred Mild)
- You’ve used them for more than 4 weeks
If any of these apply to you, your eye doctor should be checking your pressure every 1 to 2 weeks-not every month. Missing a checkup can mean irreversible damage.
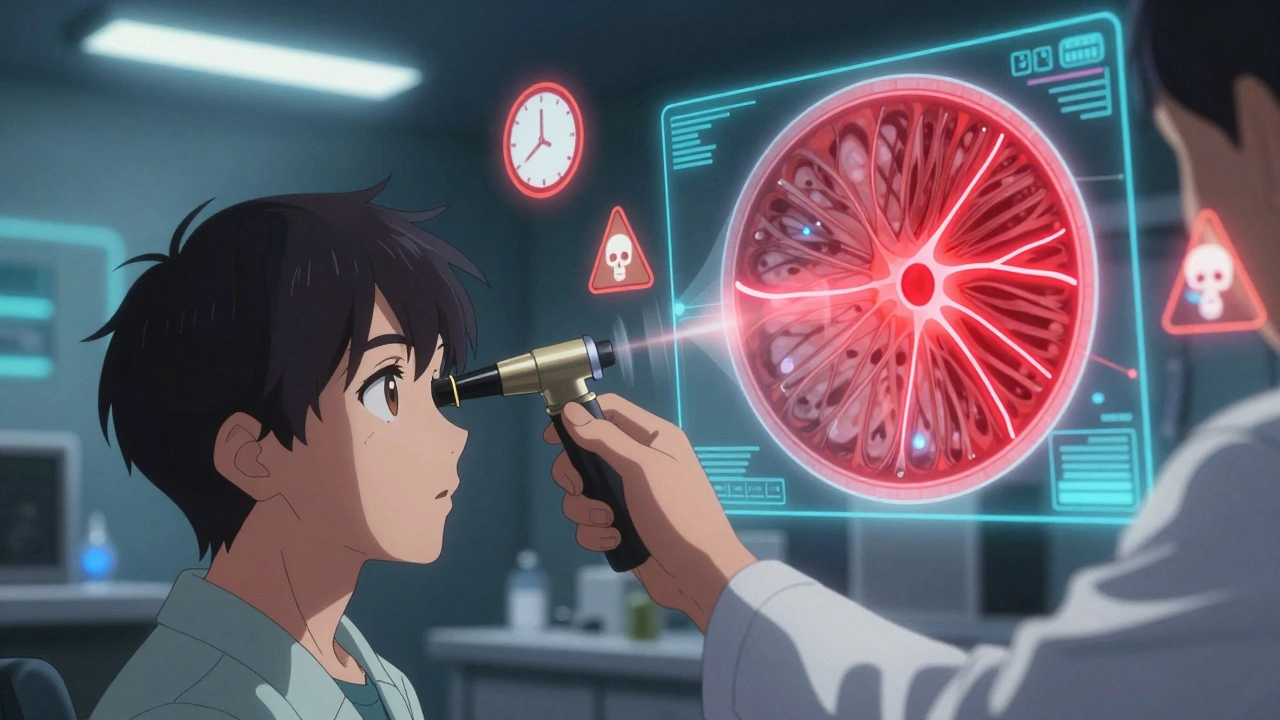
Monitoring: What Your Eye Doctor Should Be Doing
There’s no such thing as “safe” long-term steroid use without monitoring. Here’s what proper care looks like:
- Before starting: A full eye exam, including intraocular pressure (IOP) measurement with Goldmann tonometry (the gold standard), optic nerve check, and baseline visual field test.
- During treatment: Pressure checks every 2 weeks if you’re on potent steroids or have risk factors. Every 4 weeks if you’re low-risk and on a mild drop for less than 2 weeks.
- After stopping: A follow-up visit 2 to 4 weeks later to make sure pressure has returned to normal. Some patients need monitoring for months after stopping.
- For long-term users: Annual visual field tests and optic nerve imaging (OCT scans) to catch early nerve damage.
Don’t assume your optometrist knows how to monitor this properly. Ask: “Are you checking my eye pressure with Goldmann tonometry?” Many clinics use cheaper, less accurate machines. If they don’t know what you’re talking about, ask for a referral to an ophthalmologist.
When to Stop-And How to Stop
Steroid drops aren’t meant to be a long-term fix. For most conditions, 2 to 4 weeks is enough. Uveitis patients often need 1 to 2 months, but that’s the exception, not the rule.
Never stop abruptly. If you’ve used them for more than two weeks, your doctor must taper you off. Stopping suddenly can cause rebound inflammation-your eye gets worse than before. This is called “steroid rebound uveitis.” It’s painful, dangerous, and completely preventable.
Your doctor should give you a clear plan: “Use twice daily for 10 days, then once daily for 5 days, then every other day for 5 days, then stop.” Follow it exactly.
Alternatives When Steroids Are Too Risky
If you need long-term control-say, for chronic uveitis or autoimmune eye disease-steroids aren’t your only option.
Non-steroidal anti-inflammatory drops (NSAIDs) like ketorolac or bromfenac don’t raise eye pressure or cause cataracts. They’re weaker, but they’re safer for ongoing use. In some cases, doctors combine them with low-dose steroids to cut the risk.
For autoimmune conditions, oral immunosuppressants like methotrexate or biologics may be needed. These come with their own risks, but they can reduce or eliminate the need for steroid drops altogether.
There’s no one-size-fits-all. But if you’ve been on steroid drops for 3 months and your doctor hasn’t mentioned alternatives, it’s time to ask: “Is there another way?”
Symptoms That Mean You Need Help Now
You might not feel anything until it’s too late. But if you notice any of these, call your eye doctor immediately:
- Blurry vision that doesn’t clear up
- Seeing halos or glare around lights, especially at night
- Eye pain or pressure behind the eye
- Redness that comes back after the drops seemed to help
- Loss of side vision (like tunnel vision)
- Nausea or vomiting with eye pain
These aren’t “maybe” symptoms. They’re red flags. Delaying care could cost you vision.
What About Infections?
Steroids suppress your eye’s natural defenses. That means bacteria, viruses, and fungi can take hold without you noticing.
Herpes simplex keratitis is a common danger. If you’ve ever had a cold sore, you carry the virus. Steroid drops can wake it up in your eye, causing ulcers that scar your cornea. Fungal infections from contaminated drops or contact lens use are rare but devastating.
If your eye gets worse while on steroids-or if you develop a white spot on your cornea-stop the drops and get checked immediately. Never keep using them if you suspect infection.
Final Reality Check
Steroid eye drops are like a fire extinguisher. They’re life-saving when used in the right moment. But if you keep using them after the fire is out, you’ll burn down the house.
The benefits are real. The risks are serious. And the only thing standing between you and permanent vision loss is consistent monitoring. Don’t wait for symptoms. Don’t assume your doctor will catch it. Ask for pressure checks. Ask about alternatives. Ask what happens if you don’t follow up.
Your eyes don’t warn you. You have to be the one watching.

