Understanding Amiodarone and its Impact on Thyroid Function
Hey folks, Elijah here. You probably know me by now, that one bloke who loves to talk about medical intricacies and today, I'm about to take us on a journey through the world of Amiodarone and its influence on our thyroid glands. I'm your tour guide, so buckle up, and let's dive into this pool of knowledge.
Amiodarone, a medication used primarily to treat serious heartbeat irregularities could, quite paradoxically, meddle with the functioning of the thyroid gland. See, I find this fascinating, who knew tiny chemical compounds could create such a kerfuffle in the system. But hey, nothing in life is ever simple. Anyway, long story short, this interaction could be a love-hate relationship depending on your thyroid's general mood. But it's definitely worth understanding. So, no more detours. Here comes the knowledge dump.
An Introduction to Amiodarone
Let's unravel the story of this notorious but sometimes necessary guy, Amiodarone. Kicked off as a medicine specifically designed to combat serious, threatening, and irregular heartbeats, it soon rose to fame—or should I say infamy—for its interactions with the thyroid. It's worth noting that while it does play its part superbly in regulating heart rhythms, which is quite the heroic act, it can't seem to keep its hands off the thyroid. Classic case of "can't mind my own business", if you ask me.
What intrigues me is that, despite these known side effects Amiodarone continues to be a strong player in the cardiology field, purely because of its efficacy in treating serious heart conditions.
Interactions with the Thyroid
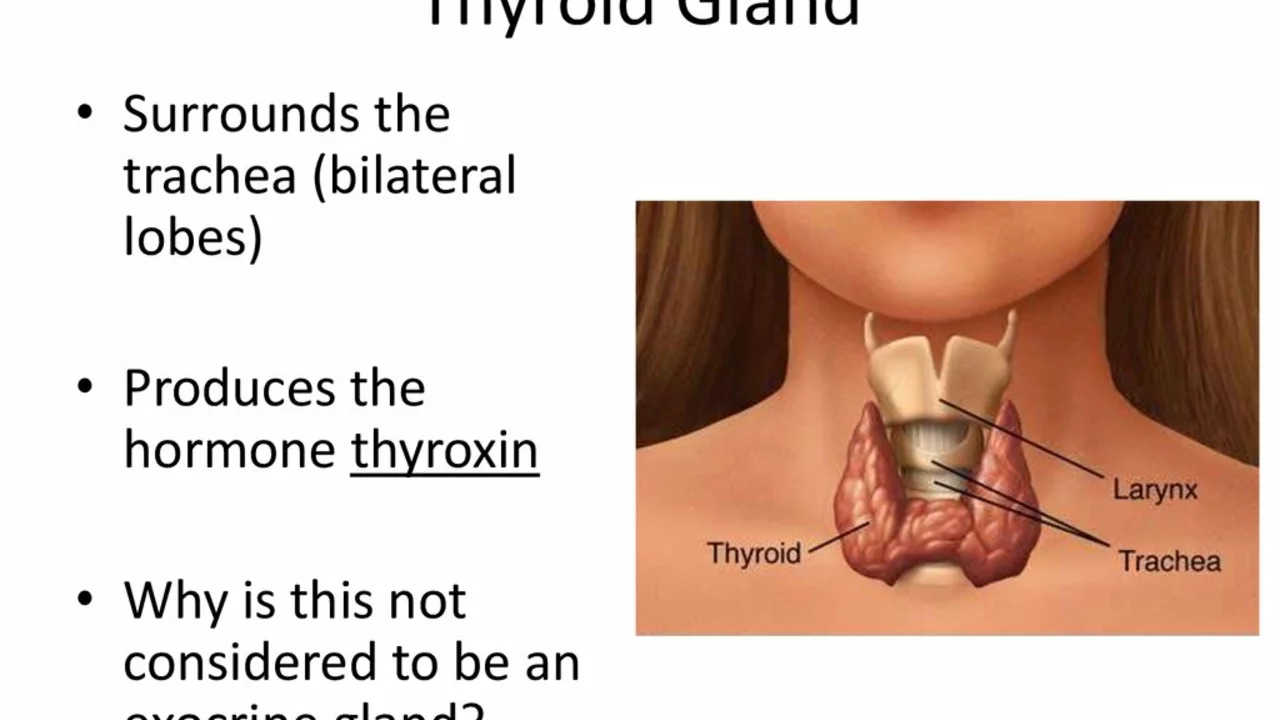
The next leg of our tour brings us straight into the thick of things - the thyroid. Our butterfly-shaped friend is incredibly impressionable, changing its behaviour based on who's around. Started hanging out with the wrong crowd? You bet! Amiodarone, with its inherent charisma, plays with the thyroid's simplicity and hijacks its usual functions.
In technical terms, Amiodarone, especially its active metabolite, desethylamiodarone, actually inhibits the enzyme thyroid peroxidase. This enzyme is in charge of converting thyroxine (T4) to triiodothyronine (T3), a process integral to our body's metabolic needs. But with big bad Amio on the loose, all this harmony goes helter-skelter!
Hyperthyroidism and Hypothyroidism: A Double Threat
The antics of Amiodarone don't just stop at creating an imbalance in the conversion process, oh no. It plays both ends of the spectrum causing a ruckus, leading sometimes to hyperthyroidism (too much thyroid hormone) and sometimes to hypothyroidism (not enough of it). It's like throwing a wrench into an already complex machinery.
This is where it gets a little more scientific. The increased iodine in the body due to amiodarone therapy can cause an overactive thyroid, or hyperthyroidism while the inhibition of thyroid peroxidase may lead to hypothyroidism. Imagine throwing a constant party and then suddenly putting a stop to it. That's what Amiodarone does to the thyroid. It's exhausting!
Diagnosis and Management of Amiodarone-Induced thyroid Disorders
Now, we're moving on to brighter pastures. Diagnosis and management - the thyroid's better half. The silver lining to this seemingly ominous tale - kind of like the little brother who always shows up just in time to get you out of trouble. These disorders, although scary, can be managed if you stand your ground, take charge, and trust your doctor's expertise. We wouldn't want to leave our thyroid dealing solo with Amiodarone now, would we?
I admit, it's easier said than done. But fret not, medications and frequent check-ins with your doctor can definitely keep these conditions at bay. So chin up, nothing's lost yet!
Lifestyle Adjustments: A Booster Shot
Now, here's my favourite part (wearing my lifestyle coach hat for a moment)—the lifestyle adjustments! These are the unsung heroes that can make a world of difference. Your diet, sleep routines, stress management, exercise, and self-care habits can be powerful tools to balance the effects of Amiodarone on the thyroid. Give yourself a chance to reconnect with your body.
The only thing worth noting here is that these changes should be introduced gradually and with a bit of patience, of course. Remember, you're not only dealing with Amiodarone but your thyroid as well. Slow and steady wins the race, and this counts doubly for the thyroid!
Cautionary Measures: Staying Ahead of the Curve
They say prevention is better than cure - now where have I heard that before? Ah yes, in every medical-related article ever. But folks, it's the truth! Taking reins of your condition, proactive checkups and adopting caution is the road very much less taken, but the one that will effectively ease your journey with this little gland.
Consider me your very own Paul Revere, warning you to get your shields up and your defenses in check. With a grain of caution, a bucket full of awareness, and your trusted doctor by your side, you've already won half the battle against Amiodarone's meddling habits with the thyroid.
Final Thoughts: The Journey Ahead
Well folks, our tour ends here, and what a ride it's been. This journey might seem a bit overwhelming but remember, amiodarone is not always your enemy. When used with due care and under supervision, it can help maintain your heart's rhythm while keeping your thyroid under control.
And as we all know, knowledge is power. With this understanding, you can stand up to the challenges posed by Amiodarone and become a champion of your own health journey. Trust yourself, live wisely, and don't forget to laugh (because remember, laughter is the best medicine!). Until next time, signing off, Elijah.