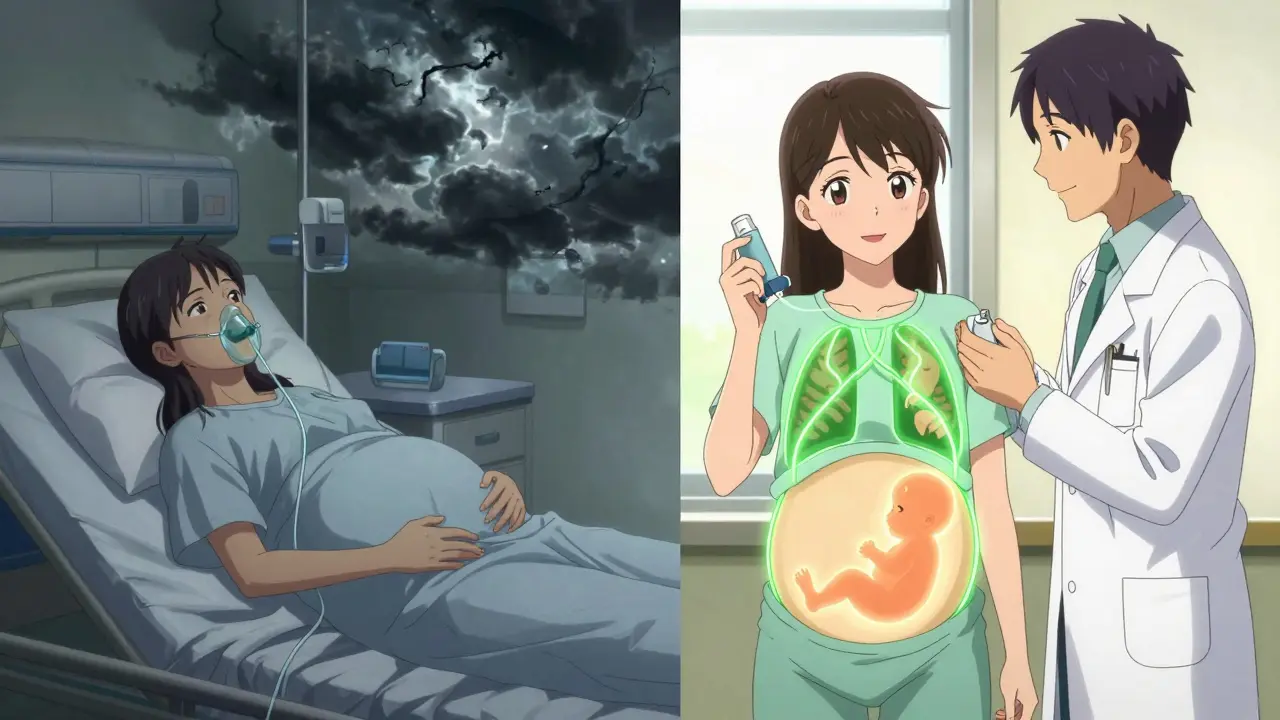
When you're pregnant and have asthma, every decision about your health feels heavier. You’re not just thinking about yourself anymore. You’re thinking about your baby too. That’s why so many women wonder: Are my asthma meds safe? Can I keep using my inhaler? Will it hurt my baby? The truth is, not treating asthma is far riskier than using the right medications.
Why Uncontrolled Asthma Is More Dangerous Than Medications
It’s easy to assume that avoiding medicine during pregnancy is the safest choice. But that’s not true when it comes to asthma. If your asthma isn’t under control, your body doesn’t get enough oxygen. And when you don’t get enough oxygen, your baby doesn’t either. That can lead to serious problems: preterm birth, low birth weight, even preeclampsia. Studies show that uncontrolled asthma increases the risk of these complications by 30% to 70%.
One large study of 1.8 million pregnancies found that women with poorly controlled asthma were 1.3 times more likely to have a baby with low birth weight. Another showed a 35% higher chance of preterm delivery. These aren’t small risks. They’re real, measurable dangers. And here’s the key point: these risks are much higher than any known risk from asthma medications when used as directed.
Doctors don’t recommend stopping your asthma meds because they’re afraid of the medicine. They recommend keeping them because they’re afraid of what happens if you stop.
The Safest Asthma Medications During Pregnancy
Not all asthma medications are created equal when you’re pregnant. The goal is to use the lowest effective dose that keeps your lungs working well - and the best way to do that is with inhaled medications. They work right where you need them: in your airways. Very little of the drug enters your bloodstream, and even less reaches your baby.
Inhaled corticosteroids (ICS) are the first-line treatment. Among them, budesonide has the most solid safety record. Over 1,000 documented pregnancies show no increased risk of birth defects. A 2021 analysis of more than 123,000 pregnancies found no link between budesonide and major congenital malformations. Beclomethasone and fluticasone propionate are also considered safe based on long-term data.
Some newer inhaled steroids, like fluticasone furoate and ciclesonide, don’t have enough pregnancy data yet. So doctors stick with the ones we know work - and that’s budesonide.
Short-acting beta-agonists (SABA) like albuterol (also called salbutamol) are your rescue inhaler. These are safe to use as needed. A review of 1.2 million pregnancies found no increase in birth defects. If you’re wheezing or short of breath, use your inhaler. Don’t wait. Delaying treatment can trigger a flare-up that’s harder to control.
Long-acting beta-agonists (LABA) like formoterol and salmeterol are only used in combination with an ICS - never alone. They’re safe for pregnancy too. Studies involving nearly 38,000 pregnancies found no increased risk of problems when used with an inhaled steroid.
Leukotriene modifiers like montelukast (Singulair) have limited but reassuring data. A European database tracking over 1,000 pregnancies found no significant rise in birth defects. Many doctors continue this medication if it was helping before pregnancy.
Medications to Avoid or Use With Caution
Some asthma treatments carry higher risks during pregnancy. The biggest red flag is oral corticosteroids like prednisone or methylprednisolone. These are powerful drugs, and while they’re sometimes necessary for severe flares, they’re not for everyday use.
A 2023 study of 1.8 million pregnancies found that taking oral steroids during the first trimester increased the risk of cleft lip or palate by 56%. There’s also a higher chance of preterm birth and low birth weight. If you need oral steroids, it’s usually because your asthma is out of control - and that’s the real problem to fix, not just the steroid use.
Theophylline is an older oral medication that’s rarely used today. It requires blood tests to make sure the dose is right, and it interacts with many other drugs. While it’s not proven to cause birth defects, it’s not the best choice when safer, easier options exist.
Long-acting muscarinic antagonists (LAMA), like tiotropium, have almost no safety data in pregnancy. Only about 300 pregnancies have been reported in databases. Until more information is available, guidelines say to avoid them as a first-line treatment.
Biologics - the newer injectable asthma drugs like omalizumab, mepolizumab, or dupilumab - are a gray area. Omalizumab has data from over 700 pregnancies with no major safety signals. But for the others, there’s simply not enough information. Most doctors won’t start these during pregnancy unless you’re already on them and doing well. Stopping them suddenly could cause a dangerous flare.
What Happens If You Stop Your Asthma Meds?
Many women stop their inhalers out of fear. But the consequences are real.
A Canadian registry tracking pregnant women with asthma found that 41% of those who stopped their inhaled corticosteroids had at least one severe asthma attack requiring emergency care. Only 17% of women who kept using their meds had the same problem.
On online forums, women often share stories of being told by well-meaning doctors or family members to “just breathe through it” or “wait until after the baby is born.” But asthma doesn’t wait. A flare-up during pregnancy can lead to hospitalization, oxygen therapy, or even ICU admission - and that’s far riskier than any medication.
One mother in Sydney told her doctor she was terrified of her inhaler. She stopped it for two weeks. Within days, she was waking up gasping for air. She ended up in the ER at 28 weeks. Her baby was born two weeks early, weighing just under 5 pounds. She didn’t need to go through that. Her asthma was manageable - if she’d kept taking her budesonide.
How to Monitor Your Asthma During Pregnancy
Managing asthma during pregnancy isn’t just about pills and inhalers. It’s about tracking your symptoms and knowing when something’s off.
Doctors recommend using a peak flow meter daily. This small handheld device measures how fast you can blow air out of your lungs. Your goal is to stay above 80% of your personal best. If you drop below 80%, it’s a warning sign. Below 70%? That’s a red flag - you may need a short course of oral steroids or a trip to the clinic.
Use an Asthma Control Test (ACT) every few weeks. It’s a simple five-question survey. A score of 20 or higher means your asthma is well-controlled. Below 20? Time to talk to your doctor. Don’t wait for a crisis.
Keep a symptom diary. Note when you wheeze, cough, or wake up at night. Track your inhaler use. This helps your doctor see patterns - like if your asthma worsens around week 24 or after exposure to pollen.
Non-Medication Strategies That Help
Medications are the backbone of asthma control, but lifestyle changes make a big difference too.
Allergen avoidance is powerful. Use allergen-proof mattress and pillow covers - they reduce dust mite exposure by over 80%. Keep indoor humidity between 30% and 50%. That stops mold from growing. Remove carpets, especially in bedrooms. They trap dust, pet dander, and other triggers.
Quit smoking - and avoid secondhand smoke. Smoking during pregnancy with asthma doubles the risk of your baby being born too early or too small.
Get your flu shot every year. Pregnant women with asthma are at higher risk for serious complications from the flu. The vaccine is safe and protects both you and your baby.
Stay active. Walking, swimming, and prenatal yoga are safe and help keep your lungs strong. Just avoid outdoor exercise on high-pollution days.

Working With Your Care Team
You don’t have to manage this alone. The best outcomes happen when your obstetrician and your asthma specialist work together.
Guidelines recommend joint check-ups at 8, 16, 24, and 32 weeks. That’s not just routine. It’s protection. Your lung function changes during pregnancy. Your medication needs might too. Regular visits mean adjustments happen before things get out of hand.
Telehealth has made this easier. Since 2020, nearly half of pregnant women with asthma now use virtual visits for follow-ups. You can send your peak flow readings, describe symptoms, and get advice without leaving home.
What About Breastfeeding?
Good news: most asthma medications are safe while breastfeeding. Inhaled steroids pass into breast milk in tiny amounts - far less than what your baby would get from the air. Albuterol, montelukast, and even budesonide are all considered compatible with nursing. You can keep using your inhalers without worry.
What’s Changing in 2025?
Research is moving fast. A major NIH-funded study launched in early 2024 is tracking 2,500 children born to mothers with asthma to see if asthma meds affect brain development or learning later in life. Early data looks reassuring, but we’ll know more by 2027.
Also, more drug manufacturers are now required to report pregnancy exposure data. That means future guidelines will be even more precise.
And the biggest shift? Doctors are finally listening. No longer are women being told to “tough it out” or “wait until after delivery.” The message is clear: your asthma matters. Your baby needs you healthy. And the right medications help you both.
Is it safe to use my inhaler while pregnant?
Yes, most asthma inhalers are safe during pregnancy. Inhaled corticosteroids like budesonide and rescue inhalers like albuterol have been studied in hundreds of thousands of pregnancies and show no increased risk of birth defects. The biggest danger is uncontrolled asthma - not the medication.
What if I had an asthma attack and needed oral steroids?
A short course of oral steroids (like prednisone) for a severe flare is sometimes necessary and safer than letting your asthma go untreated. While there’s a slightly higher risk of cleft lip or preterm birth if used in the first trimester, the risk from an uncontrolled asthma attack is much greater. Always use the lowest dose for the shortest time needed.
Can asthma medications cause birth defects?
The vast majority of asthma medications, especially inhaled ones, do not increase the risk of birth defects. Budesonide, the most studied inhaled steroid, has been used in over 1,000 pregnancies with no link to major malformations. Oral steroids carry a small increased risk if taken early in pregnancy, but that risk is far lower than the dangers of uncontrolled asthma.
Should I stop my asthma meds if I’m trying to get pregnant?
No. If your asthma is controlled, keep taking your medications. Stopping increases your risk of flares, which can affect fertility and early pregnancy. Talk to your doctor before conceiving so you can optimize your treatment plan. Many women successfully manage asthma through pregnancy without changes.
Is it safe to use a nebulizer during pregnancy?
Yes, nebulizers are safe during pregnancy. They deliver the same medications as inhalers - just in a mist form. Some women find them easier to use, especially if they’re having trouble coordinating inhaler use. Albuterol and ipratropium nebulizer solutions are both considered safe.
Will my baby inherit my asthma?
Asthma has a genetic component, so your child may have a higher chance of developing it - especially if both parents have allergies or asthma. But this isn’t guaranteed. Good asthma control during pregnancy, avoiding smoke, and breastfeeding can reduce the risk. It’s not about the meds you take - it’s about keeping your lungs healthy so your baby gets the best start.

