When you see bright red blood in your stool or on the toilet paper, it’s natural to panic. But not all lower GI bleeding is the same. Two of the most common causes-diverticula and angiodysplasia-look different, behave differently, and need very different treatments. Knowing how doctors figure out what’s going on can help you ask the right questions and avoid unnecessary tests.
What Exactly Is Lower GI Bleeding?
Lower gastrointestinal bleeding means blood coming from somewhere in your colon or rectum, not your stomach or small intestine. It usually shows up as bright red or maroon stool, sometimes with clots. People often call it hematochezia. If the blood has been sitting in the gut for a while, it can turn black and tarry (melena), but that’s more typical of upper GI bleeding. The key is: if you’re over 60 and suddenly notice fresh blood, you’re in the highest risk group.It’s not rare. About 20 to 27 out of every 100,000 people experience it each year. And the two biggest culprits? Diverticula and angiodysplasia. Together, they cause more than half of all serious cases.
Diverticula: The Silent Bleeder
Diverticula are small pouches that bulge out from the wall of your colon. They’re super common-over half of people over 60 have them. Most never cause problems. But sometimes, one of these pouches starts bleeding.Here’s how it happens: Blood vessels run right next to the inner lining of your colon. When a diverticulum forms, it pushes those vessels outward. Over time, the vessel gets stretched thin and can rupture. No inflammation. No pain. Just sudden, heavy bleeding. Some people lose a liter of blood in minutes.
That’s why it’s scary. You might be fine one minute and feel dizzy the next. But here’s the good news: about 80% of these bleeds stop on their own. No surgery. No endoscopy needed. Your body just seals it up.
Still, if you’re weak, your heart is racing, or your hemoglobin is below 10 g/dL, you need to get checked. That’s when doctors jump into action.
Angiodysplasia: The Slow Leak
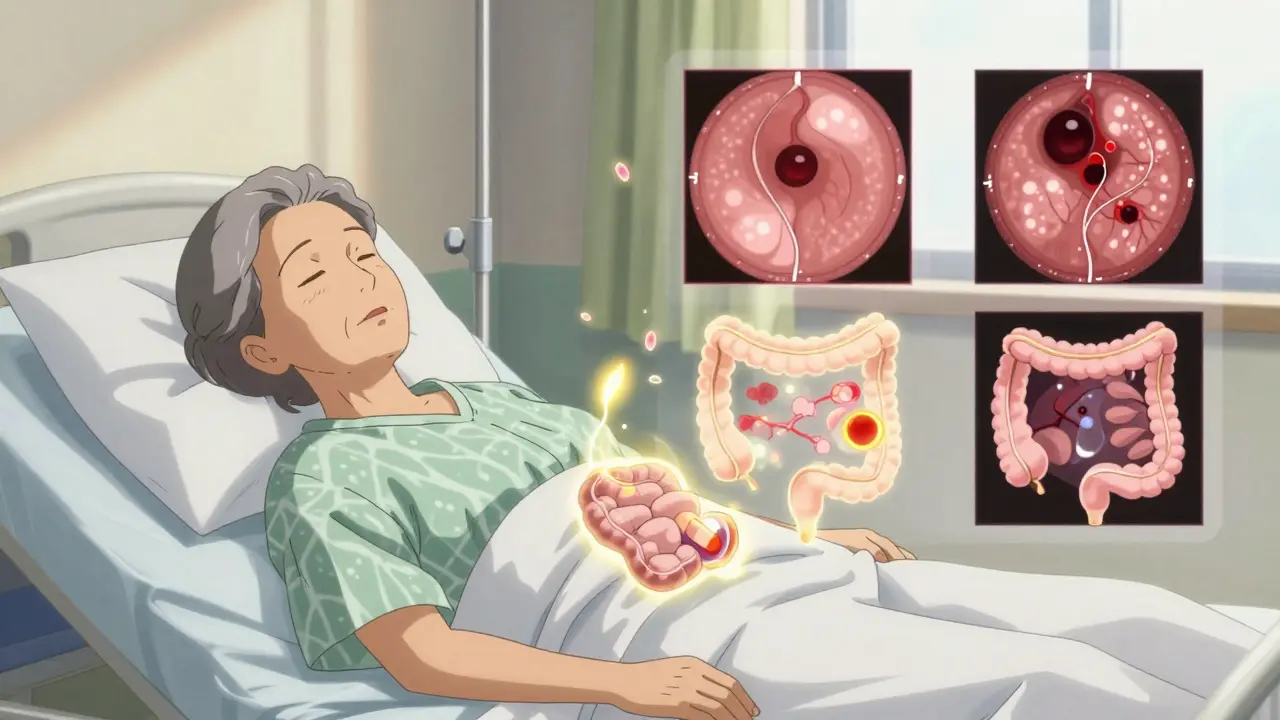
Angiodysplasia-also called vascular ectasia-isn’t a disease you get overnight. It’s a slow, age-related wear-and-tear process. As you get older, the small arteries and veins in your colon start to stretch and tangle. Think of them like old garden hoses that crack and leak over time.Most cases happen in the right side of the colon, especially around the cecum. And they’re almost always in people over 65. The average age? 72.
Unlike diverticula, angiodysplasia doesn’t bleed hard and fast. It drips. Slowly. Over weeks or months. That’s why many people don’t even realize they’re bleeding until they’re exhausted, pale, and short of breath from chronic anemia. Fatigue is often the first sign, not blood in the stool.
There’s also a sneaky link to heart disease. If you have aortic stenosis-a narrowing of the valve that controls blood flow out of your heart-the turbulent flow can damage a clotting protein called von Willebrand factor. That makes you more likely to bleed from these fragile vessels.
How Doctors Figure Out What’s Causing the Bleed
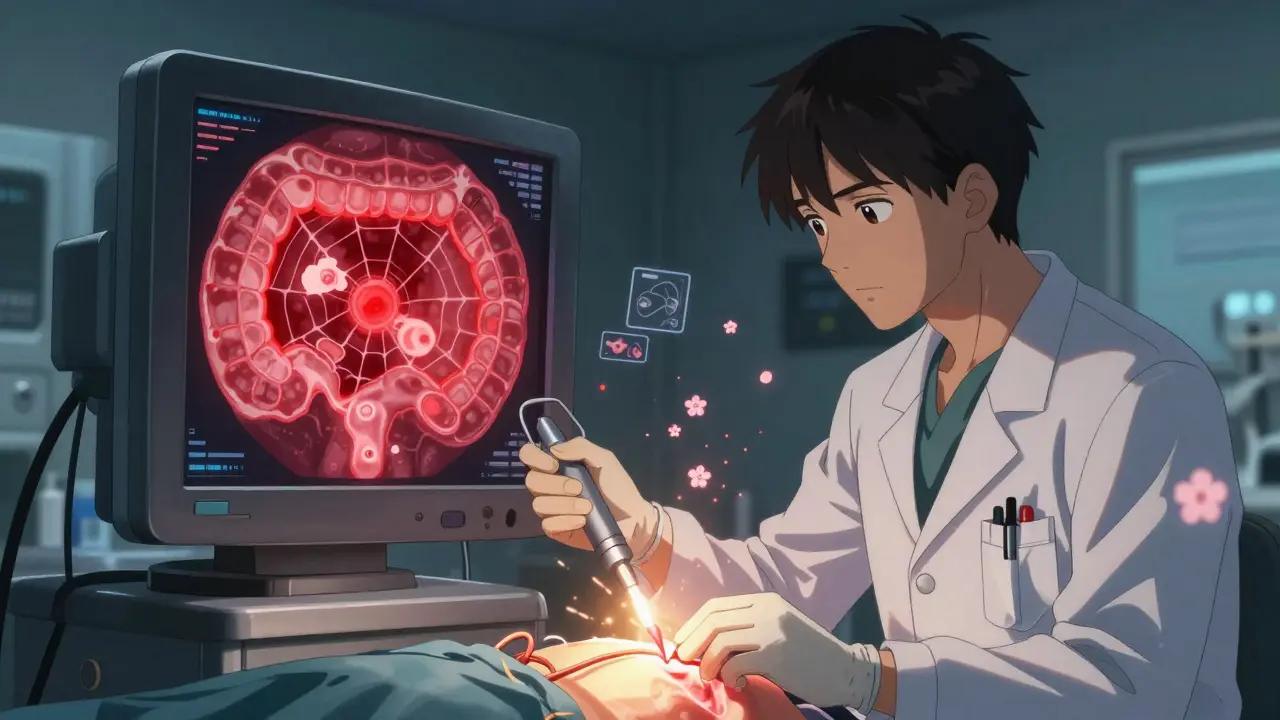
The first thing they do? Stabilize you. Check your blood pressure, heart rate, and hemoglobin. If you’re in shock, they give fluids and blood. Then they start looking for the source.Colonoscopy is the gold standard. It’s not just a diagnostic tool-it’s also the best way to stop the bleeding. Doctors aim to do it within 24 hours. Studies show that doing it early cuts death rates by 26% compared to waiting 48 hours.
You don’t need a perfect bowel prep for this. In fact, if you’re actively bleeding, they’ll skip the usual prep and use IV fluids and a drug called erythromycin. It speeds up your gut movement, so the scope can see better.
Here’s what they’re looking for:
- Diverticula: One or more pouches with a visible vessel or clot on top.
- Angiodysplasia: Red, spiderweb-like patches, often flat and subtle. They’re easy to miss without a trained eye.
AI-assisted colonoscopy is now helping. A 2022 study found it catches 35% more angiodysplasia lesions than human eyes alone. That’s huge.
What If the Colonoscopy Is Negative?
About 10-15% of people with LGIB have no obvious source during colonoscopy. That’s called obscure GI bleeding.Next step? Capsule endoscopy. You swallow a tiny camera that takes pictures as it moves through your intestines. It finds the cause in about 62% of these cases. But it’s not perfect. About 15% of people have a narrow spot in their bowel that traps the capsule. That’s why some experts say: use it only after colonoscopy.
Another option: device-assisted enteroscopy. This uses balloons to stretch the small bowel and let the scope go deeper. It finds the source in 71% of cases. But it’s complex, takes time, and isn’t available everywhere.
CT angiography is another powerful tool. If you’re still bleeding at a rate of more than 0.5 mL per minute, a CT scan with contrast can pinpoint the exact vessel leaking. It’s especially useful if you can’t have a colonoscopy due to unstable blood pressure or if the scope can’t find anything.
Treatment: What Actually Works
For diverticula bleeding:- Most cases stop on their own. Just rest, hydrate, and monitor.
- If it keeps bleeding, endoscopic therapy works. Doctors use epinephrine injections to constrict the vessel, then apply heat (thermal coagulation) to seal it. Success rate? 85-90%.
- But it can come back. About 1 in 4 people rebleed within a year. That’s why some surgeons recommend removing the affected colon segment if you’ve had two episodes.
- Argon plasma coagulation (APC) is the go-to. It’s a non-contact heat therapy that cauterizes the abnormal vessels. Immediate success? 80-90%.
- But rebleeding is common-up to 40% within two years. That’s why some patients need repeat treatments.
- For recurrent cases, doctors may try thalidomide. Sounds scary, but in a 2019 trial, 100 mg daily cut transfusion needs by 70%. It’s not FDA-approved for this, but it’s used off-label.
- Octreotide, a hormone that reduces blood flow to the gut, helps too. Given as an injection three times a day, it reduces bleeding in about 60% of patients.
- If all else fails, and the lesion is in the right colon, removing the cecum (right hemicolectomy) is often the answer.
What to Expect Long-Term
The good news? Most people recover well. The 5-year survival rate for both diverticula and angiodysplasia-related bleeding is over 80%. But survival isn’t about the bleed itself-it’s about your other health problems.Diverticula bleeding has a 10-22% 30-day death rate, but mostly because patients are older and have heart disease, kidney issues, or diabetes. The bleed itself rarely kills.
Angiodysplasia doesn’t kill as often, but it’s a nuisance. People with recurrent bleeding often describe a “diagnostic odyssey”-years of colonoscopies, negative results, and frustration. One study found patients waited an average of 18 months for a correct diagnosis.
That’s why having a clear plan matters. Hospitals that use standardized LGIB protocols-where nurses, ER docs, and gastroenterologists all follow the same steps-have better outcomes.
When to Worry (And When Not To)
Not every spot of blood means disaster. Occasional bright red streaks on toilet paper? Likely hemorrhoids. But if you’re dizzy, your heart is pounding, or you’ve passed a lot of blood in a short time-get checked.And don’t assume angiodysplasia is the cause just because you’re old. Many elderly people have incidental vascular lesions that never bleed. Treating them without proof of active bleeding can lead to unnecessary procedures.
Bottom line: If you’re over 60 and bleeding from below, get evaluated. Don’t wait. Don’t assume it’s “just hemorrhoids.” The right test, done fast, can save your life-or at least your peace of mind.
Can diverticula bleeding be prevented?
There’s no proven way to prevent diverticula from bleeding. Eating high-fiber foods helps prevent new diverticula from forming, but doesn’t stop existing ones from bleeding. Avoiding NSAIDs (like ibuprofen) may reduce risk slightly, since they can irritate the gut lining. The best approach is early detection and knowing your symptoms.
Is angiodysplasia cancer?
No, angiodysplasia is not cancer. It’s a vascular abnormality-like a leaky pipe in your colon. But because it can cause chronic bleeding and anemia, it’s often mistaken for a tumor. That’s why doctors check for cancer during colonoscopy, even when they see vascular lesions.
Why do I need a colonoscopy if I already had one last year?
Because bleeding can happen anywhere, and not all lesions are visible at once. Angiodysplasia lesions can be tiny, flat, or hidden behind folds. A colonoscopy done during active bleeding is different from a routine screening. It’s like checking for a leak while the water is running-not after it’s stopped.
Can I take blood thinners if I have angiodysplasia?
It depends. If you’re on blood thinners for atrial fibrillation or a stent, your doctor will weigh the risk of clotting against the risk of bleeding. Sometimes, they’ll reduce the dose or switch to a different medication. Never stop your blood thinner without talking to your doctor. Stopping it can cause a stroke or heart attack.
What’s the difference between diverticulitis and diverticular bleeding?
Diverticulitis is when diverticula get infected and inflamed-you’ll have abdominal pain, fever, and possibly nausea. Diverticular bleeding is when a blood vessel ruptures-no pain, just sudden, heavy rectal bleeding. They’re two different conditions, even though they come from the same pouches.

