Osteoarthritis isn't just "old age" in your joints. It’s a real, measurable disease that slowly breaks down the cushioning between bones - and it’s happening to more people than ever. By 2040, nearly 78 million Americans could be living with it. That’s one in every three adults. If you’ve felt a deep ache in your knee after walking, or stiffness in your fingers that won’t loosen up in the morning, you’re not alone - and you’re not just getting older. You’re dealing with a condition that can be managed, slowed, and sometimes even reversed in its early stages.
What’s Actually Happening Inside Your Joint?
Your joints aren’t just bones rubbing together. They’re complex systems. Cartilage, the smooth, rubbery tissue that covers the ends of bones, acts like a shock absorber. Ligaments hold everything in place. Synovial fluid lubricates the joint. Fat pads cushion and protect. In osteoarthritis, all of these parts start to break down - not just the cartilage.The process starts quietly. Tiny cracks form in the cartilage surface. Chondrocytes, the cells that maintain cartilage, go into overdrive trying to repair the damage. But they can’t keep up. The cartilage gets rough, thin, and eventually wears away. Bone begins to rub on bone. The body responds by growing bony outgrowths called osteophytes - what doctors call bone spurs. The joint lining swells. Fluid builds up. Pain follows.
Unlike rheumatoid arthritis, which is caused by your immune system attacking your joints, osteoarthritis is mechanical and biological. It’s not caused by infection or autoimmunity. It’s caused by repeated stress, injury, genetics, and metabolic changes. That’s why two people of the same age can have wildly different outcomes - one with perfect knees, another with severe pain. It’s not luck. It’s biology.
Which Joints Are Most Affected?
Osteoarthritis doesn’t hit all joints equally. The most common targets are the ones that carry weight or get used constantly:- Knees - 60% of cases. This is where pain becomes life-changing. Walking, climbing stairs, even standing up from a chair becomes a struggle.
- Hips - 30% of cases. Pain here often radiates to the groin or thigh. Many people mistake it for lower back pain.
- Hands - 25% of cases. Bony bumps at the finger joints (Heberden’s and Bouchard’s nodes) are classic signs. Buttoning shirts, opening jars, typing - all become difficult.
- Spine - 20% of cases. Neck and lower back pain, especially with stiffness in the morning, can signal OA in the facet joints.
It usually affects one side more than the other. You might have worse pain in your right knee than your left. That’s normal. It’s not symmetrical like some other forms of arthritis.
How Is It Diagnosed - And Why Is It Often Missed?
Doctors still rely mostly on X-rays to diagnose osteoarthritis. But here’s the problem: X-rays only show bone changes. By the time you see joint space narrowing or bone spurs on an X-ray, the cartilage is already badly damaged. That’s like waiting for a car’s engine to seize before you check the oil.Early symptoms are subtle: occasional stiffness after sitting, a dull ache after activity, a feeling of "grating" when you move. Many people ignore these signs or assume they’re just aging. A 2022 study found that nearly 40% of people with early OA symptoms didn’t seek help until their pain was moderate to severe.
Dr. Virginia Byers Kraus at Duke University says we need better tools - blood or urine tests that detect early cartilage breakdown products. Researchers are working on them. Until then, diagnosis is based on symptoms, physical exam, and imaging. If your pain gets worse with movement and improves with rest, and you’re over 45, it’s likely OA.

How Osteoarthritis Differs From Other Arthritis Types
It’s easy to confuse osteoarthritis with other joint problems. Here’s how to tell them apart:- Rheumatoid Arthritis (RA): Autoimmune. Pain is worse in the morning and improves with movement. Swelling is symmetrical - both hands, both knees. Often accompanied by fatigue and fever.
- Gout: Sudden, intense pain, redness, and swelling - often in the big toe. Attacks come and go. Caused by uric acid crystals.
- Post-Traumatic Arthritis: Develops after a joint injury - like a broken bone or torn ligament. Can appear years later.
Osteoarthritis is slower. It doesn’t cause systemic symptoms. It’s localized. And crucially - it’s modifiable. You can change its course.
What Actually Works for Managing Pain and Slowing Progression?
There’s no magic pill. But there are proven strategies - and they’re not what most people expect.1. Movement Is Medicine - Not the Enemy
The biggest myth about OA? That you should rest your joints. Wrong. Movement is the most effective treatment.Land-based exercises - walking, cycling, swimming, tai chi - strengthen the muscles around the joint. Stronger muscles = less stress on the joint. A 2022 Arthritis Foundation trial showed that people who did 45 minutes of exercise three times a week for 12 weeks cut their pain by 40% on average.
You don’t need to run marathons. Start with 10 minutes a day. Walk around the block. Use a stationary bike. Do chair squats. Consistency beats intensity. The goal isn’t to eliminate pain - it’s to build resilience.
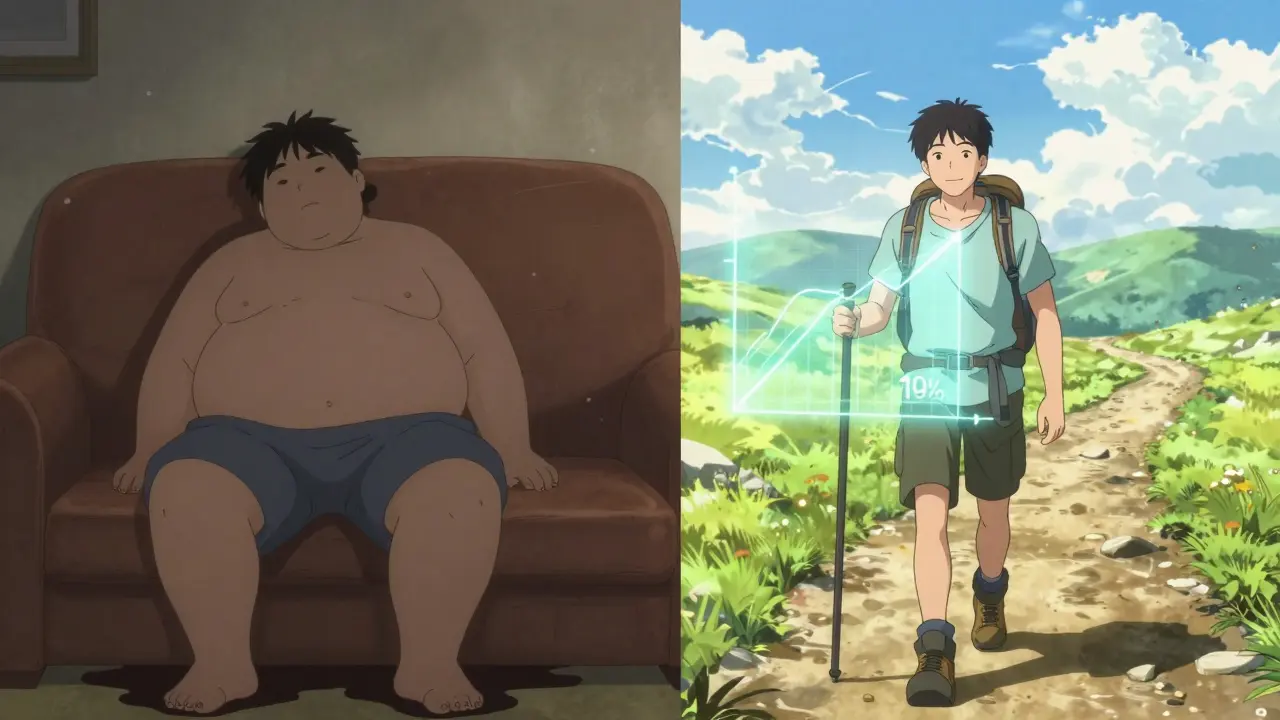
2. Weight Loss - The Most Powerful Intervention
Losing just 10% of your body weight can reduce knee OA pain by 50%. For every pound lost, you take 4 pounds of pressure off your knees.A 2023 study found that people who lost 10% of their weight and added exercise had 3 times better outcomes than those who only took medication. It’s not about being thin. It’s about reducing mechanical load. Even if you’re not overweight, losing a few pounds can make a huge difference.
3. Physical Therapy - Learn How to Move Differently
A physical therapist doesn’t just give you exercises. They teach you how to protect your joints during daily life. How to stand up from a chair without twisting your knee. How to grip a jar without crushing your fingers. How to walk without limping.Studies show that 6 to 8 sessions with a certified therapist lead to long-term improvements in function. Most insurance plans cover this. Don’t skip it.
4. Medications - Use Them Wisely
Over-the-counter painkillers like ibuprofen or naproxen (NSAIDs) help - but they’re not a long-term solution. About 32% of people stop taking them because of stomach issues, kidney strain, or high blood pressure.Topical creams with capsaicin or NSAIDs can be safer for the gut. Acetaminophen (Tylenol) helps mild pain but doesn’t reduce inflammation. For flare-ups, corticosteroid injections into the joint can give 4 to 8 weeks of relief. A 2023 update from the Osteoarthritis Research Society International confirmed this is one of the most effective short-term treatments for knee OA.
Newer drugs like tanezumab (approved by the FDA in June 2023) target nerve growth factor and reduce pain 35% more than NSAIDs. But they’re reserved for severe cases due to potential side effects.
5. Supportive Devices and Lifestyle Adjustments
A cane in the hand opposite your painful knee can reduce pressure by up to 20%. Knee braces, shoe inserts, or even a raised toilet seat can make daily life easier.Use adaptive tools: jar openers, reachers, ergonomic keyboards. Modify your home: grab bars in the shower, non-slip mats, a bench in the shower. These aren’t signs of weakness - they’re smart adaptations.
What Doesn’t Work - And What’s Still Unproven?
There’s a lot of noise out there. Here’s what science says:- Glucosamine and chondroitin: Large studies (like the NIH’s GAIT trial) show they don’t work better than placebo for most people. Some report mild benefit - but it’s not consistent.
- Stem cell injections: Still experimental. Over 380 clinical trials are running, but no standardized treatment exists yet. Beware of clinics charging thousands for unproven therapies.
- Cruciate ligament surgery for OA: If you have OA and a torn ACL, surgery won’t fix the arthritis. It might even make it worse.
- Joint replacement too early: Replacing a knee or hip before age 60 increases the chance you’ll need a second surgery later. Wait until pain and disability seriously limit your life.
Real People. Real Results.
On Reddit, a user named "KneePainSince40" wrote: "I could barely walk 10 minutes. PT and losing 18 pounds changed everything. I’m hiking again at 52." The Arthritis Foundation’s 2022 survey of 1,200 people found:- 72% improved symptoms after losing 10% of body weight.
- 68% had pain that disrupted sleep.
- 57% struggled with stairs.
- 42% couldn’t do simple tasks like buttoning shirts.
Those aren’t statistics. Those are real lives. And the common thread? People who took action - movement, weight loss, education - saw the biggest gains.
What’s Next? The Future of Osteoarthritis Care
The future is early detection. Researchers are developing blood tests that can spot cartilage breakdown products before pain even starts. Dr. Marc Hochberg predicts we’ll have these tests within five years - allowing us to intervene before the joint is damaged.Meanwhile, public health efforts are growing. The CDC’s "Active People, Healthy Nation" initiative is funding community programs in all 50 states to help people with arthritis stay active. Hospitals are starting OA education classes - 6-week programs that teach self-management. People who complete them reduce pain by 40% and improve function by 30%.
But here’s the catch: none of this matters if we don’t tackle the root causes. Obesity rates are still rising. Physical inactivity is at an all-time high. Without change, OA will keep growing - not just as a medical problem, but as a social and economic one. It already costs the U.S. $140 billion a year.
What You Can Do Today
If you have joint pain:- See a doctor. Don’t wait until you can’t walk.
- Start moving - even if it’s just 10 minutes a day.
- Track your weight. Aim for a 5-10% reduction if you’re overweight.
- Ask about physical therapy. It’s covered by most insurance.
- Learn joint protection techniques. Use tools. Modify your environment.
- Be skeptical of miracle cures. Stick with what’s proven.
Osteoarthritis doesn’t have to mean giving up your life. It means changing how you live. Not with pills and procedures alone - but with movement, mindset, and smart choices. The science is clear. The tools are available. You don’t need to suffer in silence.

