When your child grabs their ear, cries nonstop, and runs a fever, it’s hard not to panic. You’ve heard the stories: antibiotics fix ear infections fast. But what if they don’t? What if the best thing you can do is wait? Otitis media - the medical term for middle ear infection - is one of the most common reasons parents take their kids to the doctor. In fact, over 80% of children have at least one by age 3. Yet, the way we treat it is changing - and understanding why could save your child from unnecessary side effects, reduce antibiotic resistance, and help you make smarter decisions.
What Actually Happens in a Middle Ear Infection?
The middle ear is the small air-filled space behind the eardrum. It’s connected to the back of the throat by a narrow tube called the Eustachian tube. In adults, this tube works like a drain - it opens to let fluid out and air in, keeping pressure balanced. In young kids, it’s shorter, more horizontal, and doesn’t open as easily. That’s why babies and toddlers get ear infections so often.
When a cold, flu, or allergy causes swelling in the nose and throat, the Eustachian tube gets blocked. Fluid builds up behind the eardrum. That fluid isn’t always infected - but if bacteria or viruses get in, it becomes a breeding ground. That’s acute otitis media (AOM): the red, swollen, painful version. The eardrum bulges. The child screams when you touch their ear. They might have a fever, be fussy, pull at their ear, or have trouble sleeping.
But here’s the twist: not all fluid behind the eardrum means infection. Otitis media with effusion (OME) is when fluid stays after the infection clears. It’s silent - no pain, no fever. Kids might seem a bit off, or you might notice they don’t respond when you call their name. That’s because the fluid muffles sound. Hearing can drop by 15 to 40 decibels - like listening through a pillow. The good news? This fluid usually goes away on its own within three months. Antibiotics won’t help it.
What Causes These Infections?
It’s not just bad luck. Certain things make ear infections way more likely:
- Daycare attendance: Kids in group care are 2 to 3 times more likely to get ear infections because they’re exposed to more viruses.
- Secondhand smoke: Living with a smoker increases the risk by 50%. The chemicals paralyze the tiny hairs in the Eustachian tube that normally push fluid out.
- Bottle-feeding while lying down: Milk can flow back into the Eustachian tube. Breastfeeding upright reduces this risk.
- Genetics: Some kids just have anatomy that makes drainage harder.
- Season: Infections peak in fall and winter, right when colds and flu are spreading.
And the bugs? Most often, it’s Streptococcus pneumoniae, Haemophilus influenzae (non-typeable), or Moraxella catarrhalis. Viruses like RSV, rhinovirus, and flu can start it too. The same bugs that give you a stuffy nose can turn into an earache.
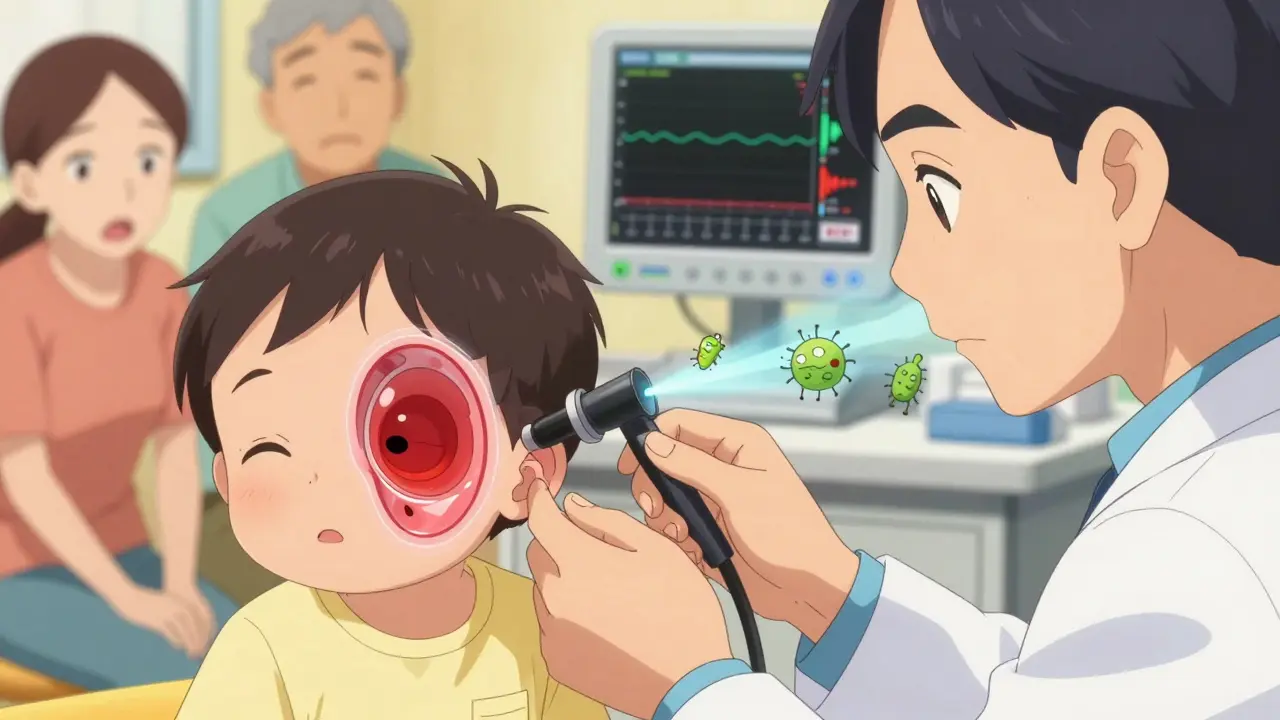
How Do Doctors Diagnose It?
It’s not just about redness. A doctor doesn’t just look - they listen. Using a pneumatic otoscope, they gently puff air into the ear. A healthy eardrum moves freely. An infected one is stiff, bulging, and doesn’t budge. That’s the key sign.
They also check for:
- Fluid behind the eardrum (cloudy or yellowish)
- Redness and swelling
- Signs of rupture (pus draining out)
Some clinics now use tympanometry - a quick, painless test that measures eardrum movement. Studies show it cuts down unnecessary antibiotic prescriptions by 22% in kids under 3. And with tools like the CellScope Oto (a smartphone attachment), parents can even take pictures of the eardrum and send them to the doctor. One study found these images were 85% accurate compared to in-person exams.
Antibiotics: When They Help - and When They Don’t
This is where things get tricky. For years, doctors handed out antibiotics like candy for ear infections. But here’s the truth: 80% of uncomplicated ear infections clear up on their own within 3 days. Antibiotics only shave off a day or two of pain. And they come with risks.
The American Academy of Pediatrics (AAP) and American Academy of Family Physicians (AAFP) updated their guidelines in 2022 to reflect this. Here’s what they recommend:
- Under 6 months: Always prescribe antibiotics. Their immune systems aren’t strong enough to fight it alone.
- 6 to 23 months: Antibiotics if symptoms are severe (fever over 39°C / 102.2°F, ear pain lasting more than 48 hours). Otherwise, watchful waiting for 48-72 hours is fine.
- 2 years and older: If symptoms are mild, wait. If severe - fever, intense pain - start antibiotics.
First-line treatment? Amoxicillin. Dose? 80-90 mg per kg per day, split into two doses. For kids under 2 with bilateral infection (both ears), it’s a full 10-day course. For older kids with mild cases? 5-7 days is enough.
What if they’re allergic to penicillin? Alternatives include ceftriaxone (a single shot), cefdinir, or azithromycin. But avoid fluoroquinolones - they’re banned for ear infections because of serious nerve and tendon risks.
And resistance? It’s real. In the U.S., 30-50% of Streptococcus pneumoniae strains are resistant to regular penicillin. But high-dose amoxicillin still works for most. Still, Haemophilus influenzae is becoming harder to treat - resistance to amoxicillin-clavulanate jumped from 7.2% in 2010 to 12.4% in 2022.
Pain Management: The Real First Step
Before you even think about antibiotics, treat the pain. That’s the priority. A child with a painful ear won’t sleep, eat, or calm down. And pain relief is what makes watchful waiting possible.
- Ibuprofen: 5-10 mg per kg every 6-8 hours. Works better than acetaminophen for ear pain.
- Acetaminophen: 10-15 mg per kg every 4-6 hours.
- Warm compress: A warm (not hot) washcloth over the ear helps soothe.
- Otic drops: Like Auralgan - but only if the eardrum isn’t ruptured. If you see pus or fluid leaking out, stop.
Parents on Reddit and parenting forums say the same thing: “Ibuprofen every 6 hours made the difference between screaming and sleeping.” That’s not just comfort - it’s the foundation of safe, smart care.
When to Worry: Red Flags
Watchful waiting doesn’t mean ignoring signs. Call your doctor or go to urgent care if your child has:
- Fever over 104°F (40°C)
- Pain that doesn’t improve after 48 hours of pain meds
- Drainage of pus or blood from the ear
- Dizziness, vomiting, or neck stiffness
- Facial weakness (one side of the face drooping)
- Signs of hearing loss lasting more than 3 months
A ruptured eardrum sounds scary - but it’s actually a relief. The pressure pops, pain drops, and fluid drains. It usually heals on its own in a few weeks. Still, it needs medical follow-up.

What About Recurrent Infections?
One in five kids gets three or more ear infections in six months. That’s recurrent otitis media. It’s frustrating - for parents and kids. Repeated antibiotics can lead to diarrhea, rashes, and yeast infections. And it fuels antibiotic resistance.
For these kids, options include:
- Ear tubes (tympanostomy tubes): Small tubes placed in the eardrum to let fluid drain. Often recommended if infections keep coming back or if hearing loss affects speech development.
- Pneumococcal vaccines: PCV13 (Prevnar 13) and the newer 15-valent Vaxneuvance have cut vaccine-type pneumococcal ear infections by 34%. Make sure your child is up to date.
- Eliminating smoke exposure: If you smoke, quitting is the single most effective prevention step.
What Doesn’t Work
Don’t waste time or money on these:
- Probiotics: A 2022 Cochrane review of 13 studies found no significant reduction in ear infections.
- Home remedies: Garlic oil, tea tree oil, or ear candles? No evidence. And ear candles can burn your child’s skin or push wax deeper.
- Antibiotics for fluid alone: If there’s no pain or fever, don’t treat. The fluid will go away.
The Bigger Picture: Why This Matters
Every year in the U.S., otitis media leads to 15.5 million doctor visits and costs over $2.89 billion. Antibiotics for ear infections make up 15 million prescriptions - the second most common reason kids get them, after sore throats.
But we’re getting better. In 2010, 68% of ear infections got antibiotics. By 2016, that dropped to 59%. That’s progress. The goal now isn’t to eliminate antibiotics - it’s to use them wisely. When they’re needed, they’re lifesavers. When they’re not, they’re a risk.
And the future? Doctors are moving toward faster diagnostics - like point-of-care tests that identify bacteria in minutes. That means we’ll soon be able to say, “This is a virus - no antibiotics.” Or, “This is resistant bacteria - we need a different drug.”
For now, the best thing you can do is stay calm, manage the pain, watch for red flags, and trust the guidelines. Your child’s ear infection doesn’t need to be fixed fast. It needs to be fixed right.
Do all ear infections need antibiotics?
No. Up to 80% of middle ear infections in children resolve on their own within 3 days. Antibiotics are recommended only for infants under 6 months, children with severe symptoms (high fever, intense pain lasting over 48 hours), or those at higher risk for complications. For mild cases in older children, watchful waiting with pain management is the preferred first step.
What’s the best medicine for ear infection pain?
Ibuprofen (5-10 mg per kg every 6-8 hours) is more effective than acetaminophen for ear pain. Acetaminophen (10-15 mg per kg every 4-6 hours) is a good alternative if ibuprofen isn’t suitable. Warm compresses can help too. Avoid ear drops if the eardrum might be ruptured - always check with a doctor first.
Can ear infections cause hearing loss?
Yes - but usually temporary. Fluid in the middle ear can reduce hearing by 15-40 decibels, making sounds muffled. This often improves as the infection clears. If fluid lasts longer than 3 months or infections keep recurring, hearing loss can affect speech and language development. In these cases, doctors may recommend ear tubes.
Is it safe to wait 48 hours before giving antibiotics?
Yes - for most healthy children over 6 months with mild symptoms. Studies show that waiting 48-72 hours doesn’t increase the risk of complications. Pain control with ibuprofen or acetaminophen is key during this time. Watch for red flags like high fever, pus drainage, or worsening pain. If symptoms don’t improve or get worse, antibiotics are still an option.
How can I prevent my child from getting ear infections?
Reduce risk by: breastfeeding upright (not bottle-feeding while lying down), avoiding secondhand smoke, ensuring up-to-date vaccines (especially PCV13 or Vaxneuvance), minimizing daycare exposure if possible, and washing hands frequently. Children in daycare are 2-3 times more likely to get infections, so consider smaller group settings if recurrent infections are a problem.

