Renal Dose Adjustment Calculator
This calculator estimates how your kidney function affects medication dosing. Your kidneys filter waste and help eliminate drugs from your body. If your kidney function is reduced, your doctor may need to adjust your dose to prevent side effects or ensure the drug works properly.
Results
Estimated Glomerular Filtration Rate (GFR): 0 mL/min
Adjusted Dose: 0 mg
Current dose: 0 mg (adjustment: 0%)
Ever wonder why a pill that works perfectly for your friend gives you a headache? Or why your doctor adjusts your dose after a few weeks? It’s not magic. It’s pharmacokinetics-the science of how your body moves, changes, and gets rid of drugs. This isn’t just for doctors and pharmacists. Understanding it helps you know why side effects happen, why some meds don’t work for you, and how to stay safer on medication.
What Happens When You Swallow a Pill?
When you take a drug, your body doesn’t just accept it like a gift. It treats it like an intruder-and tries to handle it in four clear steps: Absorption, Distribution, Metabolism, and Excretion. Scientists call this the ADME process. It’s the same for every drug, whether it’s aspirin, antibiotics, or antidepressants. First comes absorption. This is how the drug gets into your bloodstream. If you take it by mouth, it travels through your stomach and intestines. Only about 40-60% of most oral drugs actually make it into your blood. Why? Because your liver starts breaking some of it down before it even circulates. This is called first-pass metabolism. That’s why some drugs are given as injections-they skip this step and go straight in, giving you 100% of the dose. Not all drugs absorb the same way. Some need an empty stomach. Others work better with food. Your gut’s acidity matters too. Weak acids, like aspirin, absorb best when your stomach is highly acidic (pH 1.5-3.5). If you’re on acid-reducing meds, that can change how well your other drugs work.Where Does the Drug Go After It Enters Your Blood?
Once in your bloodstream, the drug starts distribution. It doesn’t just hang out in your blood. It flows to organs, muscles, fat, and even your brain. How far it spreads depends on its chemical makeup and how much it binds to proteins in your blood. Take warfarin, a blood thinner. About 98% of it sticks to albumin, a protein in your blood. That means only 2% is free to work. If another drug kicks warfarin off that protein, suddenly you’ve got way more active drug floating around. That’s how dangerous interactions happen. Doctors measure this spread with something called volume of distribution (Vd). A low Vd means the drug stays mostly in your blood. A high Vd means it dives deep into tissues-like antidepressants that settle into brain fat. That’s why some drugs take days to kick in: they’re slowly leaking out of tissues into the bloodstream.Your Liver: The Drug Factory
Next up: metabolism. This is where your liver, mostly through enzymes called Cytochrome P450 (CYP), turns fat-soluble drugs into water-soluble ones so your kidneys can flush them out. CYP3A4 alone handles half of all prescription drugs. But here’s the twist: your genes decide how fast or slow this happens. About 3-10% of white people are poor metabolizers of CYP2D6. That means codeine, which needs to be turned into morphine by this enzyme, doesn’t work for them. On the flip side, ultra-rapid metabolizers turn it into morphine too fast-risking overdose even on normal doses. Some drugs block these enzymes. Clarithromycin, an antibiotic, shuts down CYP3A4. If you take it with simvastatin (a cholesterol drug), your body can’t break down the statin. Levels spike 10-fold. That’s how you get muscle damage, even death, from rhabdomyolysis. These aren’t rare accidents. They account for 20-30% of serious side effects.How Your Body Gets Rid of Drugs
The final step is excretion. Most drugs leave through your kidneys. Your kidneys filter blood at a rate called glomerular filtration rate (GFR). Normal is 90-120 mL/min. But if you’re over 65, have kidney disease, or are dehydrated, that number drops. A GFR under 15 means your kidneys are barely working. If you don’t adjust your dose, drugs pile up like traffic jams. That’s why vancomycin, an antibiotic, can wreck kidneys in elderly patients. One case on Reddit showed a 78-year-old’s creatinine jumped from 1.2 to 3.4 mg/dL after standard dosing-because his kidney function was ignored. He needed a lower dose, not the same one as a 30-year-old. Some drugs are also cleared by bile into the gut, then excreted in stool. And guess what? Your gut bacteria can change those drugs too. New research shows 15-20% of oral drugs are altered by intestinal microbes. That’s why two people on the same pill can have totally different results.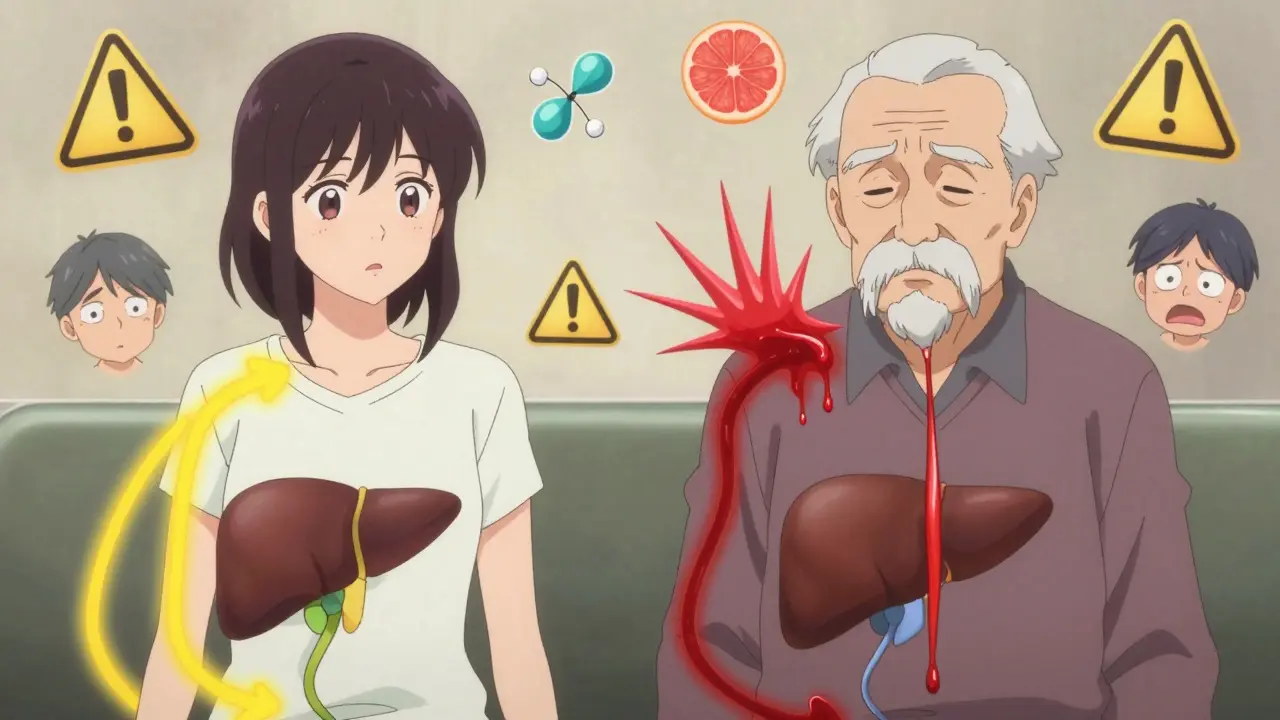
Why Side Effects Aren’t Random
Side effects aren’t just bad luck. They’re often the direct result of pharmacokinetics gone off-track. Take phenytoin, an anti-seizure drug. At therapeutic levels (10-20 mcg/mL), it works great. But if levels hit over 20 mcg/mL, 30% of patients develop side effects-tremors, slurred speech, even coma. That’s not a coincidence. It’s a direct result of too much drug hanging around because metabolism slowed down. Or consider diazepam (Valium). Its main metabolite, desmethyldiazepam, lasts up to 100 hours. In young people, it’s gone in a day. In older adults? It lingers. That’s why elderly patients feel dizzy, fall, and break hips after taking a “normal” dose. Genetics play a huge role. Warfarin users with CYP2C9 variants have a 5-fold higher risk of bleeding-even on the same dose as others. That’s why genetic testing is now required before prescribing abacavir (for HIV) and clopidogrel (for heart attacks). It’s not optional anymore. It’s standard.Age, Weight, and Other Hidden Factors
You’re not just a number on a chart. Your age, weight, liver health, and kidney function change everything. People over 65 have 30-50% less liver function and 30-40% lower kidney clearance. That’s why they’re three times more likely to have bad reactions. Yet, many prescriptions still use the same doses as for younger adults. Weight matters too. Drugs like heparin and insulin are dosed by body weight. If your weight changes and your dose doesn’t, you’re either under-dosed or over-dosed. Even what you eat can interfere. Grapefruit juice blocks CYP3A4. One glass can double the level of certain statins, blood pressure meds, and anti-anxiety drugs. That’s not a myth. It’s been proven in dozens of clinical studies.How Doctors Try to Get It Right
The good news? There are tools to fix this. Therapeutic drug monitoring (TDM) checks blood levels of drugs like lithium, vancomycin, and phenytoin. But here’s the catch: samples must be drawn within 30 minutes before your next dose. Yet, 22% of hospital labs get this wrong. That means your level might look normal when it’s actually too high. Dosing calculators like Cockcroft-Gault use your age, weight, and creatinine to estimate kidney function. But audits show 15-20% of these numbers are wrong in electronic records. If your weight is listed as 70 kg but you’re actually 90 kg? Your dose is too low. That’s why clinical pharmacists now spend 2.5-4.7 hours a week per complex patient just adjusting doses. They’re the unsung heroes preventing disasters.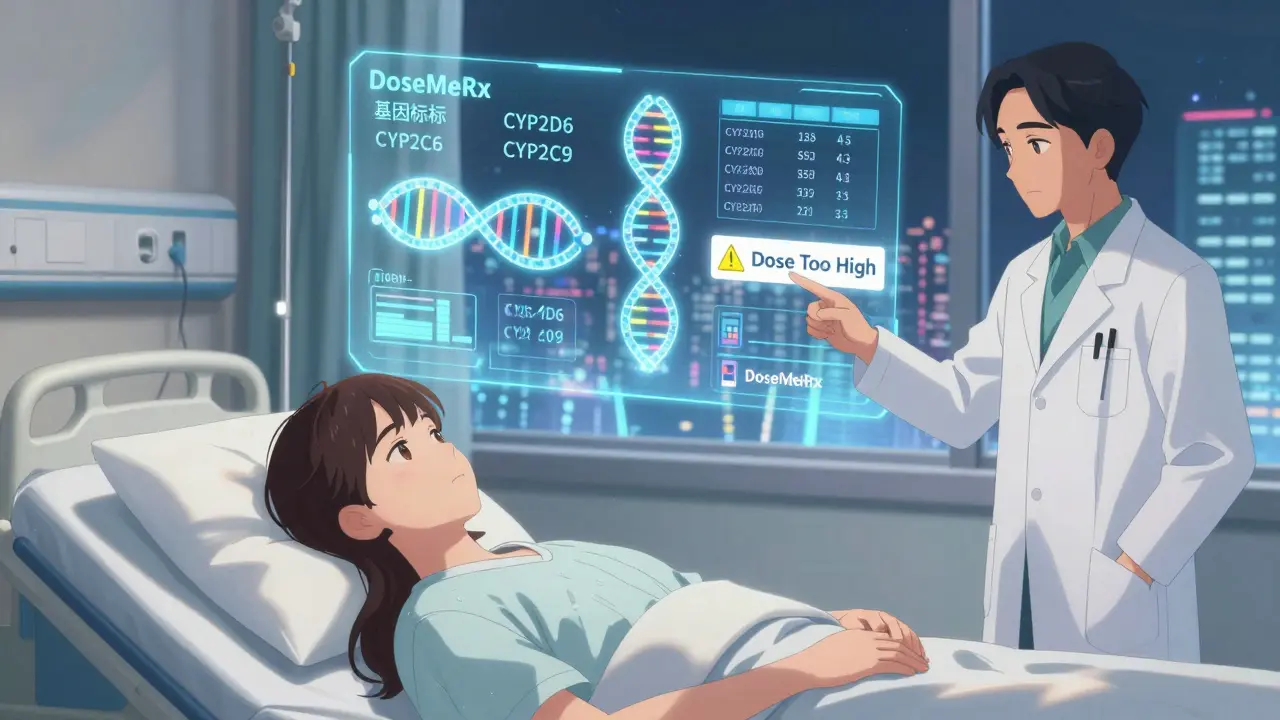
The Future: Personalized Dosing
The future isn’t one-size-fits-all. It’s one-size-for-you. AI tools like DoseMeRx now analyze your age, weight, kidney function, and genetics to suggest the perfect dose. In trials, it cut vancomycin dosing errors by 62%. The FDA approved it in 2021. The EMA’s PK4All initiative is building global databases for rare diseases-where traditional dosing fails. And the NIH is spending $185 million to fix a huge gap: 85% of pharmacokinetic studies still use young, white, male volunteers. But 85% of patients aren’t. By 2030, experts predict adverse drug reactions could drop from 6.7% to under 2% of all prescriptions. That’s 1.3 million fewer ER visits in the U.S. alone.What You Can Do
You don’t need a PhD to protect yourself.- Know your meds. Ask your pharmacist: “Is this affected by food, grapefruit, or other drugs?”
- Update your weight and kidney function in your medical records. If you’ve lost or gained weight, say so.
- Ask if you need a blood test to check drug levels-especially if you’re on warfarin, lithium, or seizure meds.
- Report side effects, even small ones. Dizziness, nausea, or fatigue might mean your dose is too high.
- Don’t assume your friend’s dose works for you. Your body is unique.
Frequently Asked Questions
What does pharmacokinetics mean?
Pharmacokinetics is the study of how your body absorbs, distributes, metabolizes, and excretes drugs. It’s often summarized as "what the body does to the drug," unlike pharmacodynamics, which is "what the drug does to the body." This process determines how much of the drug reaches its target and how long it stays active.
Why do some people have worse side effects than others?
Genetics, age, liver and kidney function, weight, and other medications all affect how your body handles drugs. For example, 3-10% of people can’t activate codeine properly due to a CYP2D6 gene variation, while others break it down too fast, risking overdose. Older adults process drugs slower, so side effects are more common.
Can grapefruit really change how my medicine works?
Yes. Grapefruit juice blocks the CYP3A4 enzyme in your gut, which is responsible for breaking down about half of all prescription drugs. This can cause drug levels to spike dangerously-especially with statins, blood pressure meds, and some anxiety drugs. Even one glass can have an effect that lasts over 24 hours.
Why do I need blood tests for some medications?
Some drugs have a narrow safety range. Too little doesn’t work. Too much causes toxicity. Medications like lithium, warfarin, phenytoin, and vancomycin require regular blood tests to make sure you’re in the safe zone. These tests are not optional-they’re lifesaving.
Are generic drugs processed the same way as brand-name ones?
Yes. By law, generics must have the same active ingredient, strength, and pharmacokinetic profile as the brand-name version. But inactive ingredients (fillers, coatings) can differ, which sometimes affects absorption-especially for drugs with tight therapeutic windows. If you switch brands and notice side effects, tell your doctor.
How can I reduce my risk of drug side effects?
Keep your medical team updated on your weight, kidney/liver health, and all medications-including supplements. Ask if your drug needs monitoring. Avoid grapefruit if you’re on statins or blood pressure meds. Never share prescriptions. And if you feel unusual symptoms, don’t ignore them-they might be your body telling you the dose is wrong.

