After a liver transplant, the biggest threat isn’t the surgery-it’s what happens next. You’re not out of the woods just because the new organ is working. The real challenge is staying alive to enjoy it. Your body sees the new liver as an invader. Left unchecked, it will attack. That’s rejection. And the only thing standing between you and graft failure is one thing: medication adherence.
What Rejection Actually Feels Like
Rejection doesn’t always scream. Sometimes it whispers. In the first few months after transplant, acute rejection is most common. It usually shows up between week one and three months. Symptoms can be subtle-or sudden.You might feel feverish, even if your temperature is only 100.1°F. That’s enough. Chills, headaches, muscle aches-these aren’t just bad flu days. They’re red flags. Pain or tenderness over your right side, where the liver sits? That’s not normal soreness. It’s your immune system trying to tear the new organ apart.
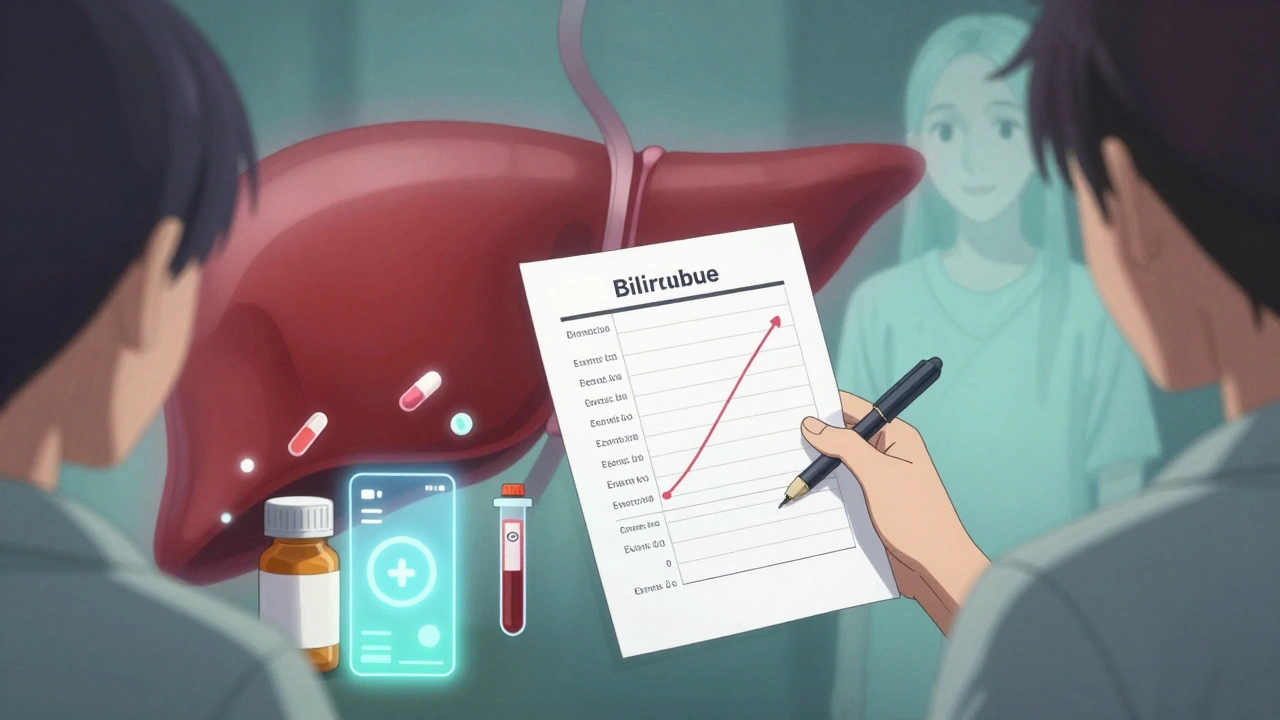
Weight gain isn’t just from eating too much. If you’ve gained 10 pounds in under 48 hours, that’s fluid building up because your liver isn’t filtering properly. Fatigue isn’t just being tired. It’s your body struggling because toxins are piling up. Yellowing skin or eyes? That’s bilirubin rising. Your liver isn’t processing it anymore.
And then there’s the blood test. Creatinine isn’t the only marker. For liver transplants, it’s bilirubin and liver enzymes-AST, ALT, ALP-that tell the real story. A jump of 20% or more in a week? That’s not normal fluctuation. That’s rejection. And it can happen even if you feel fine.
Chronic rejection is sneakier. It creeps in over months or years. Your energy slowly drains. Blood pressure creeps up. You don’t bounce back after a cold like you used to. Your liver function tests drift higher, slowly, steadily. By the time you notice, the damage is already done.
Why Missing a Dose Is More Dangerous Than You Think
You think skipping one pill won’t hurt. You were busy. You forgot. You felt fine. You thought, “I’ll just take it tomorrow.” That’s how grafts fail.Immunosuppressants like tacrolimus and mycophenolate don’t just reduce your immune response-they keep it in a fragile balance. Miss a dose, and your immune system wakes up. It doesn’t wait. It starts attacking. And by the time symptoms show up, the damage is already happening.
Studies show that missing just 20% of your doses triples your risk of rejection. That’s not a guess. That’s from the American Journal of Transplantation. And it’s not just about acute rejection. Long-term, every 10% drop in adherence means a 23% higher chance your liver will fail.
And here’s the brutal truth: many rejections are silent. You might not feel a thing. Your bloodwork might look okay. But your liver is still under attack. That’s why doctors don’t just rely on how you feel. They rely on you taking your meds-every single day, no exceptions.
The Pill Routine: More Than Just Taking Medicine
Most liver transplant patients take at least three types of drugs every day: calcineurin inhibitors (like tacrolimus), antimetabolites (like mycophenolate), and steroids. That’s often 8 to 12 pills a day, split across morning and night. Some need extra meds for blood pressure, cholesterol, or infections.Tacrolimus levels must stay between 5 and 10 ng/mL in the first year. Too low? Rejection risk spikes. Too high? You risk kidney damage, tremors, or nerve problems. And it’s not just about the dose. Timing matters. Food affects absorption. Grapefruit? Absolutely forbidden. It can spike your drug levels dangerously.
And the cost? Without insurance, annual medication runs about $28,000. That’s not a typo. Many patients skip doses because they can’t afford them. That’s not laziness. It’s desperation. But skipping meds to save money is like trading your liver for cash. The outcome is almost always worse.
How to Actually Stick to Your Meds
You don’t need willpower. You need systems.- Use a pill organizer with compartments for morning, afternoon, evening, and night. Fill it weekly. If you don’t see the pill, you won’t take it.
- Set phone alarms. Not one. Set three: 15 minutes apart. Name them: “Tacrolimus,” “Mycophenolate,” “Steroid.” Don’t just label them “Med 1.”
- Ask a family member or friend to check in every day. Just a text: “Did you take your meds?” That simple thing cuts rejection risk by nearly 30%.
- Use smart pill bottles. Some now sync with apps and send alerts if you don’t open them. Transplant centers in Sydney and across Australia are starting to hand these out. Ask your pharmacist.
- Keep a medication log. Write down what you took, when, and how you felt. Bring it to every appointment. Doctors don’t guess-they look at patterns.
Pharmacists are your secret weapon. Most transplant centers now include a transplant pharmacist on the team. They review your meds every month. They spot interactions. They help with cost. They adjust doses. Don’t wait for your doctor to ask. Go to them.
What Happens If You Miss the Signs?
If rejection isn’t caught early, you’ll need a biopsy. That’s when a needle takes a tiny piece of your liver to see if your immune system is attacking it. If it is, you’ll get high-dose steroids or stronger drugs. Sometimes, you’ll need to be hospitalized.But if it’s missed? You could end up back on the transplant list. Again. And the odds drop every time. Second transplants are harder. Survival rates fall. You’re older. Your body’s been through more. Your chances of rejection go up again.
Long-term data from the University of Pittsburgh shows this: patients who took 95% or more of their meds had an 85% chance of their liver lasting 10 years. Those who missed even 20% of doses? Only 42% made it that long.
This isn’t about being perfect. It’s about being consistent. One missed dose doesn’t doom you. But a pattern of missed doses? That’s a death sentence for your new liver.
The Future: Better Tools, Better Outcomes
The field is changing. In early 2023, the FDA approved the first genetic test for tacrolimus dosing. It looks at your DNA to predict how fast your body breaks down the drug. That means your dose can be personalized-not guessed.Some centers now use the ImmuKnow test, which measures immune activity directly. Instead of waiting for liver enzymes to spike, they see if your immune system is getting restless. It’s not everywhere yet, but it’s coming.
And then there’s the holy grail: tolerance. A small group of patients in clinical trials have been able to stop all immunosuppressants after receiving stem cell infusions alongside their transplant. Their bodies learned to accept the new liver. No drugs needed. It’s still experimental. But it’s real.
For now, though, the best tool you have is your daily routine. Your pills. Your alarms. Your log. Your support system.
You didn’t get a transplant to live with fear. You got it to live. But living means showing up-for your meds, for your checkups, for your body. Not just today. Every day.
Can I stop my transplant meds if I feel fine?
No. Feeling fine doesn’t mean your immune system isn’t attacking your liver. Many rejections happen without symptoms. Stopping meds-even for a few days-can trigger irreversible damage. Lifelong immunosuppression is the standard for a reason.
What should I do if I miss a dose?
If you miss a dose, take it as soon as you remember-if it’s within a few hours. If it’s close to your next dose, skip the missed one. Never double up. Call your transplant team immediately. They’ll advise whether you need a blood test to check drug levels.
Are there cheaper alternatives to my current meds?
Yes, but only under medical supervision. Generic versions of tacrolimus and mycophenolate exist and are often much cheaper. But switching brands can change how your body absorbs the drug. Never switch without consulting your pharmacist or transplant team. They’ll monitor your levels closely after any change.
Can alcohol or drugs affect my transplant meds?
Yes. Alcohol stresses your new liver and can interfere with how your body processes immunosuppressants. Even small amounts can raise your risk of liver damage. Street drugs are extremely dangerous-they can cause sudden organ failure. Avoid all alcohol and recreational drugs. Your liver can’t afford it.
How often do I need blood tests after the first year?
After the first year, most patients get blood tests every 1 to 3 months if stable. But if your levels have been unstable, or if you’ve had rejection before, you may need testing every 2 to 4 weeks. Always follow your team’s schedule-not your gut. Labs catch problems before you feel them.