Cancer Pain: What It Is, How It Feels, and What Actually Helps
When someone says they have cancer pain, the physical discomfort caused by cancer itself or its treatments, often persistent and complex. Also known as tumor-related pain, it’s not the same as a headache or sore muscle—it can be sharp, burning, aching, or feel like pressure deep inside. Unlike occasional pain, cancer pain doesn’t just go away with rest or ibuprofen. It lingers, changes, and often gets worse over time, especially if the cancer spreads to bones, nerves, or organs.
This kind of pain often comes with other problems: trouble sleeping, feeling hopeless, or losing appetite. That’s why managing it isn’t just about popping pills. It’s about palliative care, a focused approach to improving quality of life for people with serious illness, including pain control and emotional support. It’s not giving up—it’s taking back control. Many people don’t realize palliative care can start the same day as diagnosis. It’s not just for the end stage. And it’s not just doctors—nurses, therapists, and social workers all play a role in helping you live better while dealing with cancer.
Then there’s the medication side. opioid pain relief, strong prescription drugs like morphine, oxycodone, or fentanyl used for moderate to severe cancer pain. Also known as narcotics, they’re often necessary—but people worry about addiction, side effects, or being judged. The truth? When used correctly under medical supervision, opioids are safe and life-changing for many. They don’t make you a drug user. They let you eat, walk, talk to your kids, or sit outside without crying from pain. And they’re not the only option. Nerve blocks, physical therapy, and even certain antidepressants can help too.
Chemo and radiation can make pain worse—some drugs burn your nerves, others cause joint aches or mouth sores. That’s why knowing what’s causing your pain matters. Is it the tumor pressing on a nerve? Is it from surgery? Or is it a side effect of treatment? Each type needs a different fix. You can’t treat a burning nerve with the same pill you’d use for a broken bone. That’s why so many of the posts here focus on specific tools: how to talk to your doctor about pain levels, what to do when meds stop working, how to avoid constipation from opioids, or how to use patches, injections, or even CBD oil safely.
What you’ll find below aren’t generic lists. These are real, tested strategies from people who’ve been there. Guides on switching from one painkiller to another. Stories about what helped when nothing else did. Advice on when to push for more help and how to spot if your pain is being ignored. You’ll see comparisons between common drugs, tips for managing side effects, and even how to use non-drug methods like heat, massage, or breathing techniques that actually work.
This isn’t about hope. It’s about getting through the day without pain stealing your life. Whether you’re a patient, a caregiver, or just trying to understand, these posts give you the straight talk no one else will give you—because cancer pain is real, and you deserve to manage it well.
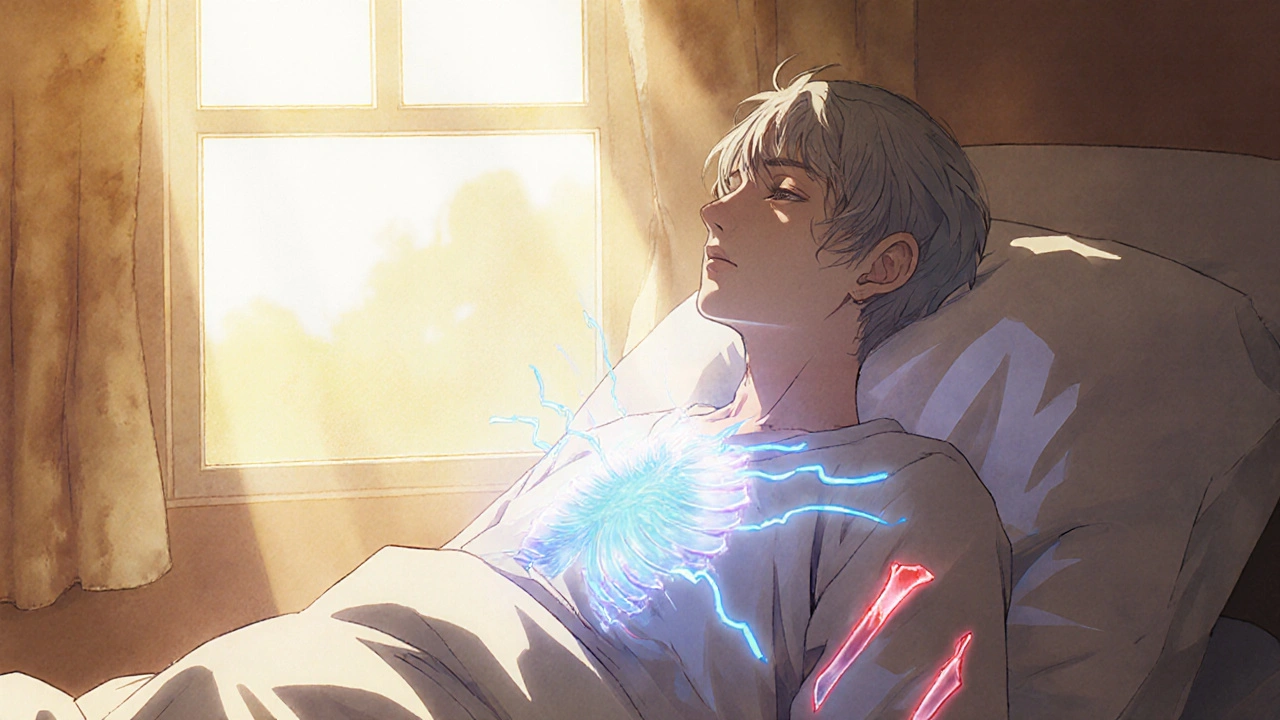
How Pomalidomide Helps Manage Cancer-Related Pain
Pomalidomide helps manage cancer pain by targeting the root causes-tumor growth and bone damage-not just masking symptoms. It's especially effective for multiple myeloma patients who haven't responded to other treatments.
