Altitude Health Risk Calculator
Every year thousands of adventurers push above 2,500 metres, only to find their bodies fighting a silent enemy. Understanding where the science is headed can mean the difference between a safe summit and a medical emergency.
What is mountain sickness and why it matters
Mountain sickness is a collective term for illnesses caused by rapid exposure to low‑oxygen environments. The most common form, Acute Mountain Sickness (AMS), presents with headache, nausea and fatigue within 6‑24 hours of ascent.
More severe conditions include High‑altitude pulmonary edema (HAPE), a fluid buildup in the lungs that can be fatal if untreated, and High‑altitude cerebral edema (HACE), swelling of the brain that leads to confusion, loss of coordination and, in extreme cases, coma.
According to the International Society for Mountain Medicine, the incidence of AMS climbs from 10% at 2,500m to over 60% above 4,500m. HAPE and HACE are rarer but responsible for most high‑altitude fatalities.
Why research is taking off now
Three forces are accelerating progress:
- Growing participation in high‑altitude tourism, with a 25% increase in trek bookings worldwide since 2020.
- Advances in wearable sensor technology that make continuous monitoring feasible on the trail.
- A surge in funding from agencies like the World Health Organization (WHO) and the National Institute of Health (NIH) targeting hypoxia‑related disorders.
These trends mean researchers can enroll larger, more diverse cohorts and test interventions in real‑world settings.
Next‑generation diagnostic tools
Early detection is the holy grail. Traditional diagnosis relies on subjective symptom scoring, which can miss silent hypoxia. New tools promise objective, real‑time data.
- Wearable pulse oximeter patches now sit on the upper arm and stream blood‑oxygen saturation (SpO₂) to a smartphone app every minute. In a 2024 field trial in the Andes, the devices identified 18% of AMS cases before symptoms appeared.
- AI‑driven predictive models analyze SpO₂ trends, heart‑rate variability and ascent speed to generate a risk score. The model developed by the University of Zurich achieved 92% accuracy in forecasting HAPE onset.
- Portable ultrasound scanners, once bulky, are now suitcase‑size. Researchers use them on Everest’s South Base Camp to spot early lung fluid accumulation, allowing immediate treatment.
Integration of these tools into a single “altitude health dashboard” is already being piloted in Nepal’s trekking industry.

Pharmacological breakthroughs on the horizon
Acetazolamide has been the mainstay for AMS prevention for decades, but its side‑effects - tingling, frequent urination and altered taste - limit tolerability. Emerging drugs aim to target the underlying hypoxia pathway more precisely.
- Dexamethasone remains the rescue drug for HACE, but new glucocorticoid analogues are in PhaseII trials that promise fewer metabolic impacts.
- Hypoxia‑inducible factor (HIF) stabilizers, originally developed for anemia, are being repurposed. Early data from a 2023 Chinese study showed that a low‑dose HIF‑PHD inhibitor reduced AMS incidence by 30% without significant adverse events.
- Gene‑editing approaches using CRISPR‑Cas9 aim to enhance the expression of endogenous erythropoietin. While still experimental, a 2025 mouse model demonstrated a 40% increase in oxygen‑carrying capacity at simulated 5,000m altitude.
These pharmacological avenues could shift the focus from symptom management to physiological adaptation.
Non‑pharmacological innovations reshaping treatment
Technology isn’t limited to pills. Devices that mimic the pressure of lower altitudes are gaining traction.
- Portable hyperbaric chamber units, weighing under 30kg, can be inflated with a foot‑pump and provide 0.5atm of pressure, enough to reverse early HAPE symptoms on the trail.
- Battery‑powered oxygen concentrators now deliver up to 2L/min of supplemental oxygen for up to 12hours, a game‑changer for remote expeditions where cylinder resupply is impossible.
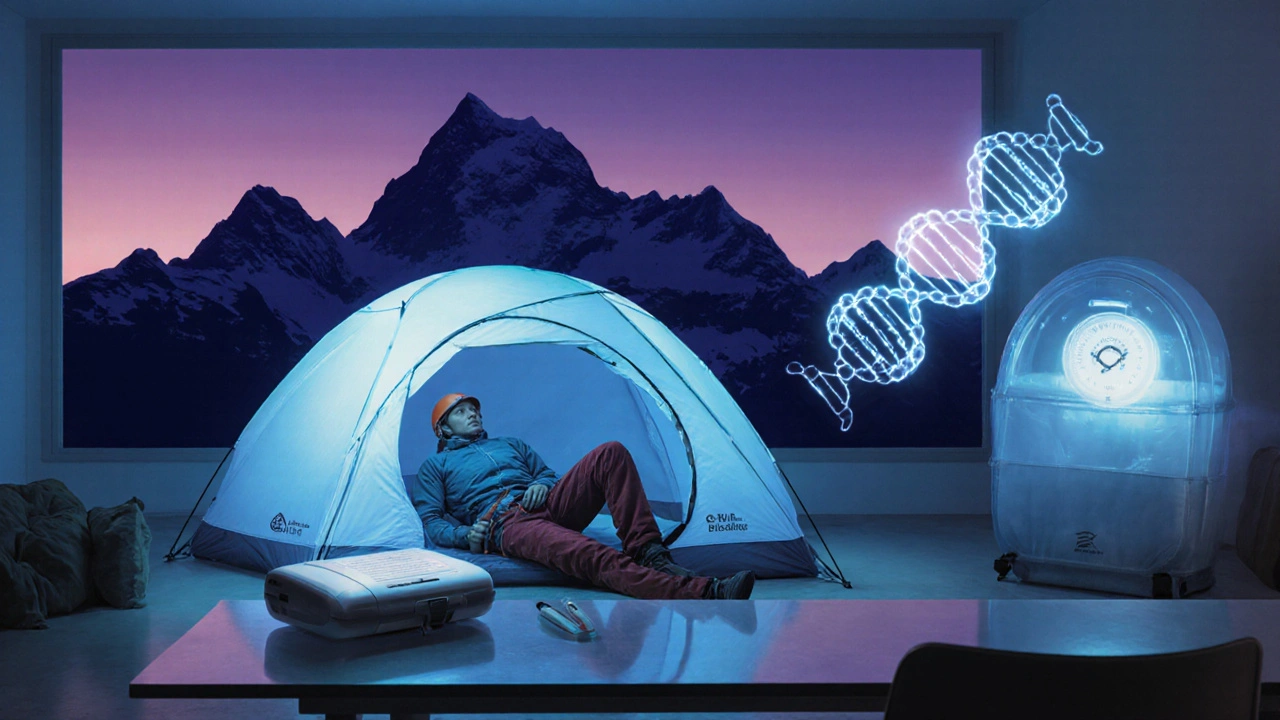
- Pre‑acclimatization protocols using hypoxic tents allow climbers to simulate altitude at home. Recent meta‑analysis of 12 trials showed a 22% reduction in AMS severity when climbers spent at least 8hours per night in a 2,500m simulated environment for three weeks.
When combined with real‑time monitoring, these tools create a feedback loop: detect early hypoxia, intervene with oxygen or pressure, and adjust ascent plans accordingly.
Personalized medicine: genetics meets the summit
Not everyone reacts to altitude the same way. Studies have identified genetic variants in the EPAS1 and EGLN1 genes that correlate with better oxygen utilization. In a 2024 Tibetan cohort, carriers of the EPAS1 “high‑altitude adaptation” allele were 45% less likely to develop AMS.
Future travel clinics may offer a simple saliva test to flag high‑risk individuals, allowing tailored prophylaxis - perhaps a lower dose of acetazolamide or a pre‑emptive HIF stabilizer. The concept of a “genetic altitude passport” is already being discussed at the International Mountain Medicine Congress.
Global collaboration driving momentum
Large‑scale studies require pooling data across continents. The WHO’s “Altitude Health Initiative” launched in 2022, now connects research sites in the Himalayas, Andes, Alps and Rockies. Through a shared database, investigators can compare outcomes of different interventions, standardize diagnostic criteria, and accelerate regulatory approval.
Funding bodies are responding. The NIH’s “Hypoxia and Human Performance” grant program awarded $25million in 2024 to projects exploring AI diagnostics, portable hyperbarics and novel drug candidates.
Practical takeaways for anyone heading upward
- Start slow: gain at least 300m of altitude per day above 2,500m, and include a rest day every 1,000m.
- Consider a pre‑acclimatization plan using a hypoxic tent or spending a night at moderate altitude before the main ascent.
- Use a wearable pulse oximeter that alerts you when SpO₂ drops below 85% for more than 30 minutes.
- If you’re prone to AMS, discuss acetazolamide or emerging HIF stabilizers with a travel clinic well ahead of the trip.
- Carry a portable hyperbaric chamber or a lightweight oxygen concentrator if you’ll be in remote areas where rescue might take hours.
- Know the early signs of HAPE and HACE - persistent cough, breathlessness at rest, confusion or loss of coordination - and descend immediately if they appear.
Adopting these strategies, backed by the latest research, turns a risky climb into a managed adventure.
Comparison of Current Standard Treatments vs Emerging Options
| Aspect | Current Standard | Emerging Option |
|---|---|---|
| Pre‑vention | Acetazolamide 125mg BID | Low‑dose HIF‑PHD inhibitor (oral) |
| Rescue for HACE | Dexamethasone 4mg IV/PO | Next‑gen glucocorticoid analogue |
| HAPE Management | Immediate descent + supplemental O₂ | Portable hyperbaric chamber + AI‑guided O₂ dosing |
| Monitoring | Symptom checklists | Wearable pulse oximeter + AI risk score |
| Personalization | One‑size‑fits‑all dosing | Genetic testing‑guided prophylaxis |
Frequently Asked Questions
How quickly can mountain sickness develop after ascent?
Symptoms of Acute Mountain Sickness often appear within 6‑24hours of reaching a new altitude, but early hypoxia can be detected by wearable oximeters before you feel any headache or nausea.
Is acetazolamide still the best preventive drug?
Acetazolamide remains effective for most travelers, reducing AMS risk by roughly 60%. However, new HIF stabilizers are showing comparable protection with fewer side‑effects, and they may become the first‑line choice once approved.
Can a portable hyperbaric chamber replace descent?
For early HAPE, a portable chamber can quickly raise ambient pressure and improve oxygenation, buying time for evacuation. It is not a substitute for descent in severe cases, but it can prevent the condition from worsening.
Do genetic tests really predict susceptibility?
Tests that identify EPAS1 and EGLN1 variants can flag individuals with a higher natural tolerance to hypoxia. While they don’t guarantee protection, they help clinicians customize prophylaxis strategies.
What role does AI play in preventing altitude illness?
AI models analyze continuous sensor data (SpO₂, heart rate, ascent speed) to generate a real‑time risk score. When the score crosses a threshold, the app prompts the user to rest, descend, or start supplemental oxygen, potentially averting severe illness.

