Amiodarone: what it does and why you should pay attention
Amiodarone is a strong antiarrhythmic used for serious heart rhythm problems like atrial fibrillation and life‑threatening ventricular arrhythmias. It can work when other drugs fail, but it has more side effects and special monitoring needs than most heart medicines. If you’re starting it, or caring for someone who is, know the main risks and the checks that keep treatment safe.
How it’s used and how it’s taken
Doctors often start with a short higher “loading” dose to reach effective levels quickly, then switch to a lower daily maintenance dose. Amiodarone comes as tablets and IV. Because it stores in tissues, it stays in the body for weeks to months after stopping — that’s why side effects can pop up even after you stop the drug. Take it exactly as prescribed; don’t skip doses or stop suddenly without talking to your doctor.
Key side effects and what to watch for
Pulmonary toxicity: the most serious risk. New or worsening cough, shortness of breath, or unexplained fever needs immediate medical review — pulmonary fibrosis can be permanent. Thyroid problems: amiodarone can cause both hypothyroidism and hyperthyroidism. Expect baseline thyroid tests and regular checks. Liver effects: your doctor will check liver enzymes; significant rises may require stopping the drug. Skin and eyes: common issues include photosensitivity and a blue‑gray skin tint on sun‑exposed areas; corneal deposits can cause blurry vision or halos but usually don’t harm sight permanently.
Other warnings: IV amiodarone can cause low blood pressure or slow heart rate. It’s generally avoided in pregnancy and breastfeeding because it crosses the placenta and affects the fetus. Carry a list of your medicines — amiodarone interacts with many drugs.
Interactions to know right away: warfarin (often need to lower warfarin dose by about a third to half), digoxin (doctors usually cut the digoxin dose roughly in half), and certain statins (avoid high doses of simvastatin or lovastatin; your doctor will pick safer options). Also avoid combining it with other drugs that dangerously slow heart rhythm or prolong the QT interval.
Monitoring plan you can expect: baseline ECG, thyroid and liver blood tests, and a chest X‑ray. After starting, thyroid and liver tests are commonly checked every 3–6 months; report new cough, breathing trouble, jaundice, fainting, or vision changes immediately. Eye checks are done if you notice vision problems.
Alternatives exist — other antiarrhythmics or catheter ablation may be safer depending on your condition. Ask your cardiologist why amiodarone is the best choice for you, how long they expect you to stay on it, and what monitoring schedule they recommend.
Bottom line: amiodarone can save lives, but it demands respect. Stick to follow‑up tests, watch for red‑flag symptoms, and keep everyone involved in your care informed about all medicines you take.
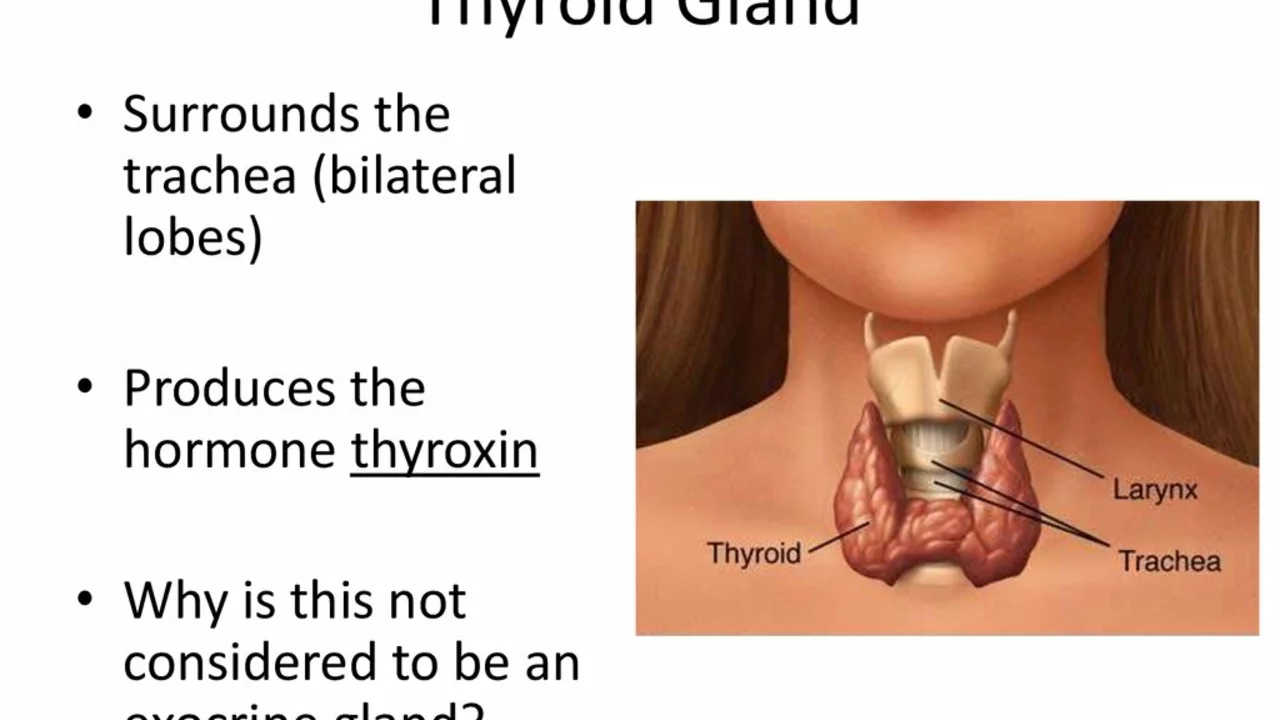
Amiodarone and Thyroid Function: What You Need to Know
Alright folks, let's dive into the wild world of Amiodarone and Thyroid Function! So, this drug, Amiodarone - it's a bit like that unexpected guest who not only crashes your party but also messes with your home's heating system, in this case, your thyroid function. It's an effective treatment for serious heart rhythm problems, but it could potentially lead to either an overactive or underactive thyroid. So, you see, it's a bit of a 'naughty medicine' - working wonders for your heart but potentially stirring up a storm in your thyroid. But hey, don't worry, your doctor is like your personal weather forecaster, monitoring any changes and helping you navigate through it. It's a crazy ride, isn't it? Buckle up, because understanding your body is like exploring a fascinating, unpredictable universe.
