Organ Transplant Survival: What Affects Long-Term Outcomes and How to Improve Them
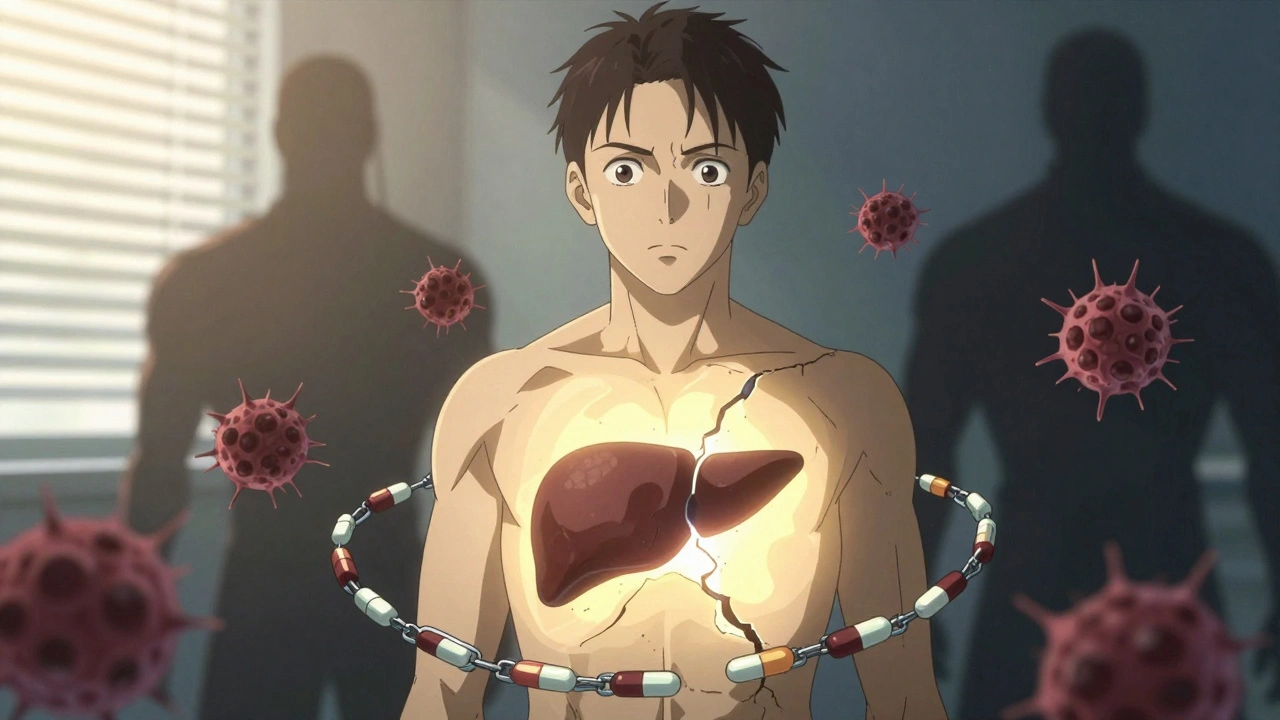
When someone gets a new organ, the surgery is just the beginning. Organ transplant survival, the likelihood that a transplanted organ continues to function over time after surgery. Also known as graft survival, it’s not just about the match—it’s about what happens next. Many people assume the transplant is the finish line, but for most, it’s the starting point of a lifelong routine. The body’s immune system doesn’t see the new organ as a gift—it sees it as an invader. That’s why immunosuppressants, medications that lower the body’s natural defense response to prevent organ rejection become non-negotiable. Take them wrong, skip a dose, or mix them with the wrong herb or food, and the organ can start failing—even years after a successful transplant.
Rejection isn’t always dramatic. Sometimes it creeps in silently, with no pain, no fever, just a slow drop in function. That’s why regular blood tests, biopsies, and doctor visits aren’t optional. Transplant rejection, the immune system’s attack on the donated organ can happen at any time, but the highest risk is in the first year. After that, the danger shifts from acute rejection to chronic damage caused by long-term drug side effects, high blood pressure, or diabetes. These aren’t just side effects—they’re part of the trade-off. The same drugs that save the organ can damage the kidneys, raise cholesterol, or increase cancer risk. That’s why post-transplant care isn’t about one drug or one test—it’s about managing a whole system. Lifestyle matters too. Smoking cuts survival time in half. Not exercising? That’s another risk. Even something as simple as avoiding grapefruit can make a difference, because it interferes with how your body processes key medications.
And it’s not just the patient. The organ donor, the person who gives a kidney, liver, heart, or other organ after death—or sometimes while alive plays a role too. Organs from younger donors, or those without a history of high blood pressure or diabetes, tend to last longer. But even with the best donor, success depends on how well the recipient follows their plan. There’s no magic pill for long-term survival—just consistency. Take your meds. Show up for your appointments. Eat real food. Move your body. Avoid infections. These aren’t suggestions. They’re the difference between living 5 years and living 20.
What you’ll find below are real, practical posts from people who’ve lived through this. From how immunosuppressants interact with herbal supplements, to why skipping a dose can trigger rejection, to how vaccines work after a transplant. These aren’t theory pieces. They’re the kind of advice you wish you’d heard before you left the hospital. This is what organ transplant survival really looks like—not in brochures, but in daily life.
Post-Transplant Life: Recognizing Rejection Signs and Staying on Track with Medication
Learn the real signs of liver transplant rejection and why sticking to your medication schedule is the single most important factor in long-term survival. No fluff. Just what works.
