Post-Transplant Care: What You Need to Know About Medications, Risks, and Daily Management
When you or a loved one undergoes an organ transplant, the surgery is just the beginning. Post-transplant care, the ongoing medical and lifestyle management required after receiving a new organ. Also known as transplant follow-up, it’s the difference between survival and rejection, between feeling normal and being stuck in the hospital. This isn’t a one-time checkup—it’s a lifetime commitment to taking pills, watching for warning signs, and making smart choices every single day.
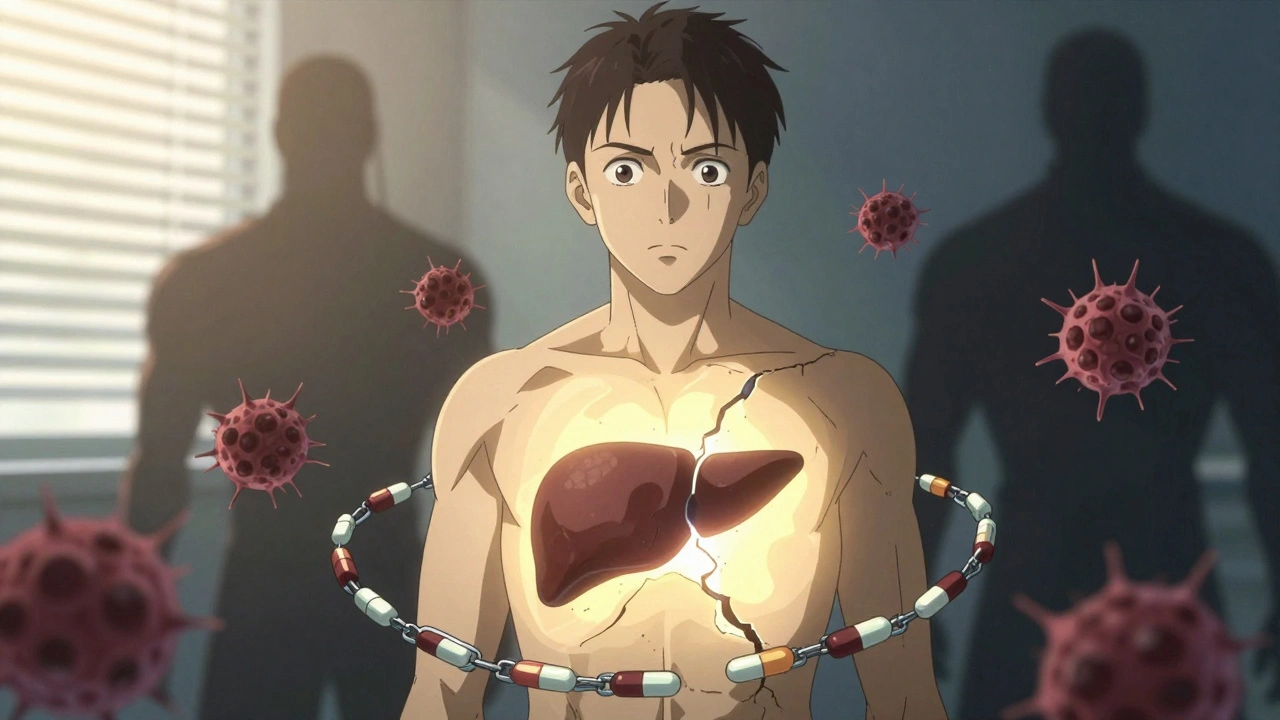
At the heart of post-transplant care are immunosuppressants, drugs that prevent your immune system from attacking the new organ as if it were an invader. These aren’t optional. Skip a dose, and your body might start rejecting the kidney, liver, or heart you were given. But these drugs come with trade-offs: higher risk of infections, kidney damage, diabetes, and even certain cancers. That’s why monitoring blood levels, tracking side effects, and never switching meds without your transplant team’s approval is non-negotiable. Many patients don’t realize that even herbal supplements like St. John’s wort or ginkgo can interfere with these drugs—leading to dangerous drops in drug levels or toxic buildup. Your pharmacist isn’t just filling prescriptions; they’re part of your safety net.
Post-transplant care also means learning to spot early signs of trouble. A fever that won’t break, unexplained swelling, sudden weight gain, or changes in urine output could mean rejection is starting. It’s not always dramatic—sometimes it’s just feeling "off." That’s why regular blood tests, imaging, and biopsies are part of the routine. And while you’re managing meds, you’re also managing your life: diet, exercise, sleep, stress. You can’t go back to old habits. No more skipping meals, no more ignoring high blood pressure, no more thinking "I’ll take the pill later." Your new organ doesn’t care about your schedule—it only cares if you’re consistent.
There’s also the emotional side. Anxiety about rejection, guilt over relying on a donor, depression from constant medication routines—these are real. And they’re not talked about enough. You’re not weak for feeling this way. You’re human. That’s why support groups, mental health check-ins, and open conversations with your care team matter just as much as lab results.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit built from real patient experiences and clinical data. You’ll read about how steroid eye drops can sneak up on you after transplant, why switching to a generic immunosuppressant can be risky, how vaccines work (or don’t) when you’re on immunosuppressants, and how to avoid dangerous drug interactions with supplements. Every post here answers questions you didn’t know to ask—because in post-transplant care, the smallest oversight can have the biggest consequences.
Post-Transplant Life: Recognizing Rejection Signs and Staying on Track with Medication
Learn the real signs of liver transplant rejection and why sticking to your medication schedule is the single most important factor in long-term survival. No fluff. Just what works.
